Posts in Category: Pet Tips
Thursday Is National Check the Chip Day
Like most pet owners, I can’t imagine the horror of having my pet lost or stolen. It’s scary and difficult to think about someone finding my little Sadie and having no way to contact me! That’s why, when she was a puppy, I had her microchipped. I wanted to take every precaution to bring her back home in the event we are separated.
I have personally witnessed many dogs and cats that were separated from their owners. I’ve seen the fear and confusion in their eyes. They seem to be wondering where they are, why they are surrounded by strangers, and how they will ever can get back home to the familiar faces and smells.
Then, with a quick scan and phone call, they are back with their loved ones, happy as can be and spoiled rotten again!
Happy endings like these are why microchips are so important for your pets. I have heard so many owners voice their regret at not having their pets microchipped, which is why I urge all of you to have it done. Microchips don’t eliminate the value of a collar or ID tag, but they can make a huge difference when it comes to reuniting lost pets with their families.
A common misconception I hear about microchips is that they are like a GPS. This is not the case. You cannot track a microchip. Rather, when the microchip is scanned, you can obtain information about the pet (usually by contacting the manufacturer who has the registration information).
For this reason, it is very important to keep the registration information accurate. If you move or change your contact information, you should contact the microchip manufacturer to update your pet’s information.
Below are some facts about microchips, provided by the American Veterinary Medical Association (AVMA) and the American Animal Hospital Association (AAHA). With support from HomeAgain, these organizations established and publicized “Check the Chip Day,” celebrated on August 15.
- 1 in 3 family pets will get lost
- Only 6 out of 10 microchips are registered
- Microchipped dogs are more than twice as likely to be returned to their owners
- Microchipped cats are more than 20 times more likely to be returned to their owners
And now some happy successful reunion news: To date, HomeAgain has reunited more than two million pets with their owners, including a dog named Gidget, that was found in Portland, Ore., more than 2,500 miles from her home in Pittsburgh, Pa., and a cat in California named George that was reunited with his family after 13-year separation!
Celebrate “Check the Chip Day” by:
- Making an appointment for microchipping, if your pet isn’t already microchipped. (Then make sure that your pet’s chip is immediately registered.)
- Checking the accuracy of your already-microchipped pet’s registration information in the microchip manufacturer’s database.
- Updating your pet’s microchip registration information if needed.
Please visit this AVMA website for additional information about Check the Chip Day, including a list of microchip manufacturers included in the AAHA Universal Pet Microchip Lookup Tool:
I hope I have convinced all of you how important it is to have your pet microchipped! If you have any questions about what having a microchip placed entails, if you would like us to check your pet for a microchip, or if you would like to schedule an appointment to have a microchip placed, please contact us.
—Amber Slaughter, DVM
Grain Free Food: Naming Names, Not Playing Games
It was about a year ago that the solemn and simple veterinary world became unstably chaotic regarding the Holy Grail of things your aunt’s neighbor recommended for your dog: Grain-Free Food.
The innocent early days of 2018 were carefree and loose, with the veterinary world throwing out lines like “There’s no reason to be on a grain-free diet, but it does no harm.” Owners were happy. Dogs were happy. Your aunt’s neighbor was happy. We left work on time.
And then, as a slow, brooding cello tremolo intensified from below, the FDA and AVMA issued statements about what they had determined was a specific correlation between grain-free food and heart disease.
You can relive the splendor in my August 2018 blog post or directly from the source: https://www.fda.gov/animal-veterinary/news-events/fda-investigation-potential-link-between-certain-diets-and-canine-dilated-cardiomyopathy
Recently, to celebrate the anniversary, the FDA has come out swinging with the names of brands that they had previously only hinted at being at the root of the problem. As the calls come pouring into the clinic for all dogs on these foods, I will try to break down the new news, though this isn’t really new at all. There have been some updates over the last year so I will try to summarize.
First, let’s get the awkward first-date questions out of the way.
What are the brands implicated?
Here are the grain-free food brands and the number of dog deaths linked to their food.
| Acana | 67 |
| Zignature | 64 |
| Taste of the Wild | 53 |
| 4Health | 32 |
| Earthborn Holistic | 32 |
| Blue Buffalo | 31 |
| Nature’s Domain | 29 |
| Fromm | 24 |
| Merrick | 16 |
| California Natural | 15 |
| Natural Balance | 15 |
| Orijen | 12 |
| Nature’s Variety | 11 |
| NutriSource | 10 |
| Nutro | 10 |
| Rachael Ray Nutrish | 10 |
No one specific protein source was identified as the problem. Cases included raw food, semi-moist food, wet food, and dry kibble.
Second, wait … what? What do you mean deaths, what?
Here is a good question-and-answer page from the FDA: https://www.fda.gov/animal-veterinary/animal-health-literacy/questions-answers-fda-center-veterinary-medicines-investigation-possible-connection-between-diet-and
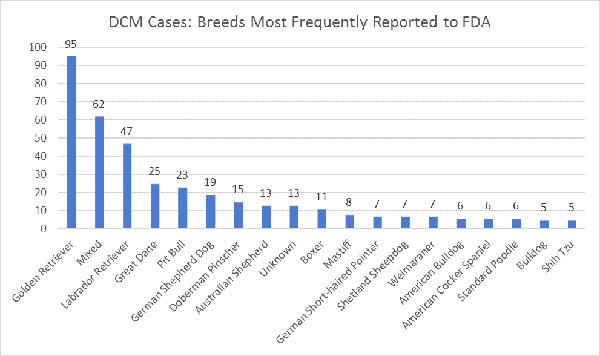
There have been 524 reports of dilated cardiomyopathy (imagine the heart enlarging like a balloon) between 2014 and 2019, and the majority of these occurred in the past 6 months. The United States has about 77 million pet dogs, so this is a small percentage, but these numbers reflect an increase in, most importantly, dog breeds not genetically likely to have dilated cardiomyopathy. (Breeds with a genetic predisposition to DCM include Doberman Pinschers, great Danes, boxers, and Irish wolfhounds.)
There is still a lack of understanding of what is going on. The early worries were that it was related to taurine deficiency, but almost all of the indicted food contained proper levels of taurine. Golden retrievers, specifically, are suspected to contract DCM due to taurine deficiency, but still, no exact information as to how this relates to grain-free diets.
The majority of implicated diets were high in legumes (peas, beans, chickpeas, soybeans, lentils, peanuts) and potatoes, which are generally used to replace the grains. (Rice is a grain, not a legume. Leave rice out of this.)
Third, what should you do?
Let’s be really clear here that 524 deaths is a very low number, but this situation is still very scary, because the FDA is still not sure why these deaths are occurring and how the diet and the deaths are linked. The grain-free-ness may not be the problem, but we just don’t know.
If your dog is dependent on a certain food listed above, it may not be the specific aspect of the lack of grain that is causing the optimal results of a diet, but something else that could be found in a different diet (for example, fiber content). We cannot tell you that you need to switch off of grain-free food, or that you have to drop your allegiance to the brands listed above, but until we know what is doing this, there is some risk.
I do not give my dog a grain-free diet, but I also do not have a dog with any gastrointestinal issues. That being said, grain-allergies are just not a thing in dogs, and, it could be concluded, feeding a grain-free diet is not worth the risk.
Please talk to us if you have questions, and of course, if your dog is suffering from lethargy, weakness, coughing, exercise intolerance, increased respiratory rate/effort, or anything that seems abnormal, please let us know.
Brett Grossman, DVM
Medical District Veterinary Clinic
The Fearful Patient: Steps to Reduce Stress
What are you terrified of? If I were to ask our staff that question, I would get a number of them telling me they are terrified of spiders. If I were to force these staff members to be exposed to spiders, they would likely scream and cry. They would do whatever they could to remove themselves from that situation.
Additionally, the more I expose them to spiders, likely the more extreme their reaction will become. Fear does not fade away with exposure but likely gets worse. Would their behavior be justified? Would they be acting irrationally?
Now I would like you to consider your cats and dogs. What are they afraid of? When they are scared, how do they behave?
Here is a small list of stressors that I have witnessed on a daily basis over many years of working in the veterinary field.
Cats:
- Transportation in a carrier
- Leaving their home environment
- Unfamiliar people
- Restraint
- Loud unknown noises and smell of dogs
- Nail trims
- Injections
Dogs:
- Unfamiliar dogs and people
- Loud noises (fireworks and thunderstorms)
- Restraint
- Nail trims
- Injections
Steps to Reduce Fear
At Medical District Veterinary Clinic, we understand that fear and stress in our patients can become dangerous for them and us. We strive to make veterinary visits less stressful for you and your pets and thus safer for everyone involved. At each visit we assess the fear of our patients and consider what we can do to decrease their stress levels.
Some of our common practices to attempt to decrease stress for cats include:
- Placing feline patients directly into one of our feline only rooms so they are not in lobby potentially with loud, barking dogs
- Allowing cats to come out of their carriers on their own. Pulling or dumping a cat out of a carrier creates a lot of stress and fear for cats.
- Removing the top of the carrier if cats do not want to exit carrier on their own and performing exam while cat remains in the bottom of the carrier, if possible.
- Using towels to help restrain, so cats can hide their face during exams
- Using feline appeasing pheromones in the exam rooms and feline hospitalization ward to decrease stress
- Prescribing medications to be given at home to decrease the stress involved with being placed in a carrier and traveling in the car
- Full sedation is occasionally recommended when it is safer for the cat and us. We feel bad for our patients that have such severe fear and anxiety in a veterinary clinic that they react in fearful/aggressive ways. The use of sedation makes their experience much more pleasant and safer for everyone involved.
Some of our common practices to alleviate stress for dogs include:
- Treats, treats, and more treats! We use a combination of dog treats and high value treats like peanut butter and cheese. I also recommend coming in when your dog is hungry so the treats are even more valued. You can also bring some treats from home if your dog has a favorite.
- Allow dogs to greet us when they feel comfortable versus quickly approaching a scared dog
- Minimal restraint techniques
- Performing most exams on the floor. Dogs do not like to be placed on tables. The really small dogs are hard to examine on the floor, so some dogs are placed on tables, but whenever possible we prefer to do exams on the floor.
- Placing alerts on patient records of dogs that are reactive with other dogs so they can be placed directly in exam rooms upon entry to the clinic. Minimizing their exposure to other dogs helps keep them calm.
- Prescribing medications to be given at home to decrease the stress involved with travel and veterinary visits
- As with highly fearful cats, dogs that have such severe fear and anxiety that they react in fear-based aggression are occasionally recommended for examination under full sedation. Sedation makes their experience less stressful and safer for everyone.
Ask for Help
Please ask any of the doctors or staff if you have questions about decreasing fear and anxiety for your dog or cat. Whether their fears are related to veterinary visits, grooming visits, thunderstorm anxiety, or something else, we would be more than happy to discuss possible alternatives and or sedatives that may be beneficial.
The mental health of our patients is important. We understand that if dogs and cats hate going to the vet, the experience is also stressful for you, and the chance of these pets getting regular veterinary care decreases. Please let us know how we can help you have a more enjoyable veterinary experience, and we will do the same.
Drew Sullivan, DVM
Medical District Veterinary Clinic
Gauging Aging: 4 Reasons You Shouldn’t Overlook Your Pet’s Signs of Slowing Down
 It’s April in Chicago, and the 10 to 15 minutes of “spring” we experience every year is bound to occur at any time.
It’s April in Chicago, and the 10 to 15 minutes of “spring” we experience every year is bound to occur at any time.
With this renewal comes all the hope laid waste by winter’s pet owner oppression. We can recall all those long walks with our dogs that did not occur due to arctic blasts. We notice the winter weight gained by our cats, who did not move from the radiator. Suddenly our hopes are renewed, and we fully intend to find a pet-friendly cabin in Michigan where we can go on a dog- and cat-family-filled hiking/poetry/organic healing retreat. (It will happen some day!)
And during this upheaval of salt-stained front hallway floors, we also start to notice changes in our pets that may have been masked by the winter’s inactivity. This is when we so often find that our beloved 6-year-old Golden and 8-year-old tortie are just not moving like they used to.
We open the windows, and our cats hesitate to jump up to smell the lilacs outside. We let our dogs off-leash in the backyard, and they run like bonkers for 15 seconds and then are just a little calmer than they’ve ever been before.
Informed of a pet’s decreased energy, hesitancy to jump, and changes in normal activity, most veterinarians would have concern. Generally though, clients will deemphasize this issue when in the exam room, saying something like, “They’re doing great! Slowing down a bit, but we know that they’re getting older.”
I think the desire to downplay our animals’ signs of aging relates to, first, a reluctance to spend money to address these signs, and second, the pain of facing our animal’s mortality. Having trouble dealing with signs of aging is normal; we do it with our own doctors as well. But there are valid reasons for taking these changes—whether subtle or pronounced—seriously.
1. Discomfort can be fixable, regardless of how small, part one
Think of how often we go to the doctor because of minor aches and pains, or we take non-prescription over-the-counter medications to help with backs, necks, knees, etc. Even at an early age dogs and cats often start to get mild arthritis (though it may often go undiagnosed) in the lower back, knees, elbows, necks, etc. Certain orthopedic issues, such as hip dysplasia, can start as early as puppyhood and progress slowly or rapidly over time.
Joint supplements can help, sometimes in dramatic ways and sometimes in ways that are harder to discern. Omega 3 fish oil and glucosamine chondroitin are the most common ones we use, but there are many others. These supplements also come mixed into foods that are, unfortunately, typically labeled for “seniors” or “joint health.” Supplements are a really good place to start to address achy joints.
The supplement industry is relatively unregulated, so before you buy Super Joint Flex Multiverse Power to the Pup Volcano Energy tabs, please check with us. Most of these supplements are non-prescription, but we have (at least, I have) opinions. The thing about inflammation, though, is that to slow its progression, supplementation must begin early. I have no problem with starting a 3-year-old cat (especially one that is prone to be heavier) on joint supplements now, rather than wait until the pain is more obvious and stifling and the supplement is correspondingly less effective.
2. Discomfort can be fixable, regardless of how small, part two
When it comes time to discuss pain medications, most clients will do almost anything to avoid starting something that may be a lifetime therapy. That being said, there’s no way to know if it will be a lifetime therapy without starting it to see if it works.
There are medications that are very and immediately effective and work on top of joint supplementation. These include anti-inflammatories, neuro-modulating drugs, and in some cases, opioids. Dosages vary from (everyone’s favorite) “as-needed” to multiple times a day.
I’ve had patients who start one or two types of medications, and the owners report seeing their pets start to act “like a puppy [or kitten]” again. We then try to wean down and find the right dose that fits the problem and specific health status of that particular animal. Sometimes this requires ruling out other conditions first, but sometimes it doesn’t.
My favorite vet-related outcome of prescribing pain medications is when clients who had assumed that their pet was too old to do a favorite thing (get in the lake, play with the laser toy, etc.) see the pet return to doing the favorite thing. Sometimes all it takes to achieve this result is a cheap, low dose of a safe drug. This is not cheating, or a shortcut to being a good owner, which I hear often. It’s just making our pets more comfortable.
3. Discomfort can be fixable, regardless of how small, part three
Along with all the options above, there are some good physical therapy facilities and caretakers in Chicago. I don’t generally go to this without trying other options first, but it is possible that with such therapy, we can avoid drugs completely or reduce the amount of drugs given in total. Some of these facilities offer relief through cold laser therapy, building back muscle strength with underwater treadmills, acupuncture, and so on. I’ve had some dogs (and cats) that we assumed had reached their end point for quality of life but gained substantial boosts in comfort from physical therapy. Again, each cat and dog is unique, so this isn’t one-therapy-fits-all.
4. This can be indication of more serious issues
Even though you are just now noticing clinical signs of aging, the signs may have been progressing for weeks or months. You’d be surprised how often something very serious can occur with a dog and cat and they just absorb it, not showing much outward indication of pain.
Dogs rupture their cranial cruciate ligaments all the time, and sometimes that fact doesn’t become obvious until months later. Cats can do this too. More commonly, cat have severely loose kneecaps that worsen over time.
Cats and dogs get mild disc disease, spinal arthritis, and other conditions that need serious therapy, which may or may not include surgery. It’s always sad to find out that a dog or cat that has been painful for months, albeit slowly and progressively, could have been made more comfortable sooner with a procedural fix or additional medications. And many times the prognosis and cost correlate with how fast we can identify the problem.
Although this article focuses on orthopedic issues, there are many neurologic, endocrine/chemical, or general systemic illnesses that first appear looking like the classic “just slowing down.” A quick exam can sometimes quickly differentiate between serious problem and normal aging. I won’t go down the path of worst-case scenarios, but dogs and cats that come to us for “slowing down for the past three months” often wind up with serious diagnoses.
I don’t mean to force everybody with a dog and cat that is getting older to worry that normal aging is a sign of having a brain tumor, but consider what you would tolerate in your own body. Getting older is not a reason for dogs to be uncomfortable. Even the healthiest dogs and cats that have never had any issues are going to need more attention, more veterinary care, and more consideration when they are 10 than they did when they were 5. This is just how life works. Luckily, with your help and attention, we can help them live as comfortably as possible for as long as possible.
Be well. Consider your choice of baseball team wisely.
Brett Grossman, DVM
Medical District Veterinary Clinic
The Free of Grain but Broken-Hearted
There are very few variables in caring for your dog that are more controllable and personal than the diet you chose for him or her. This general topic evokes very heated emotions, and there are (figuratively) billions of topics to address as subsets of diet-related controversies. For now, though, I want to write about the latest developments in grain-free food and the load of information leaking out on the Internet about its correlation with heart-related canine disease. It’s, yet again, another light and breezy summer post with which to cozy up next to your loved ones.
Here’s the Breakdown
A recent well-respected study showed a fairly well-correlated link between heart disease (dilated cardiomyopathy, or DCM) and grain-free diets, especially in breeds at higher risks, such as golden retrievers, Doberman pinschers, boxers, Irish wolfhounds, and Great Danes. There is not yet a clear understanding as to why this is the case, but the correlation is clear enough that cardiologists are steering their patients away from grain-free diets.
Some have speculated that the grain-free diets have insufficient taurine levels causing a taurine deficiency, a known cause of DCM, but even that is unclear. A few specific brands were mentioned in these studies, but the only clear commonality is that they were grain-free and legume-based (a plant that is part of the pea-family: alfalfa, clover, peas, beans, chickpeas, lentils, etc.).
On August 10, the United States Food and Drug Administration issued a statement regarding its investigation into this matter.
For Now:
First, do not panic.
If you have your dog on a grain-free diet, the safest and easiest thing to do is to stop that diet and go back to the debauchery of the pre-grain-free days of dog food. Given that there still is not much evidence of the benefits of going grain-free, the risks outweigh the supposed benefits for now. The veterinary community is working with the FDA to figure out the problem, so we may get answers soon, but until then: Well, I would switch. I am switching, literally, right now, for my dog. Most effects of taurine deficiency (and thus the correlative effects of a grain-free diet) are reversed when the diet is changed back and the deficiency is reversed.
If you have a reason to continue feeding a grain-free diet, please feel free to discuss it with us. Make an appointment and we will go over this with you. Then, we can refer you to a cardiologist for an echocardiogram to make sure there is not already an issue, and we can sample taurine levels and, if they are problematic, give taurine supplementation. We can also just start to supplement with taurine, which is fairly inexpensive. The only thing to remember is that we still are not sure if the taurine is the actual problem, so you would be taking some risks.
Because I Know You (Yes, YOU!) Are Going to Ask…
- There is a bit of a grain-free myth out there. Food allergies are fairly uncommon, and allergies to grain are even more uncommon within the subset of rare allergies. You can find accusations of grain causing cancer, still births, arthritis, the multitude and intensity of flatulence, and just about anything else. There is, as of yet, no clear correlation with grain and anything bad. I know people who swear that their dog stopped having all clinical signs of [ anything ] after going on a grain-free diet, and I believe them, but I also may put factors in the mix other than the grain. I know dogs in the wild do not eat grain, but they also do not sleep in temperature-controlled waterbeds wearing footsie pajamas.
- I hear many people discuss how they do not trust the big pet food companies. Usually the words, “cancer” and “conspiracy” are thrown out as a consequence of using their products.
I am not asking you to support Exxon brand dog treats, but I also suggest that you think about how much testing of nutritional adequacy is done with companies that can afford to do such, versus some companies that cannot. I am absolutely not suggesting that all smaller dog food brands are bad, or not to be trusted, but the foods most implicated in these studies were all made by smaller companies without a long track record of maintaining proper nutritional control over their foods. So maybe until we know the cause of this problem, you may want to stick with a brand of food that addresses this specific problem on their website or in person. If they have no answer, then maybe take a break in your relationship and go to a brand that does. The Tufts Veterinary Clinical Nutritional service lists nine questions you should be asking of the companies that make your dog’s food.
- I have had numerous emails about this topic over the last few months, and I have somewhat answered most of them with a “let’s wait and see.” So the “wait and see” is over. If I told you something different before this blog, my new answer is: Switch food.
- There has been absolutely no indication that grain-free cat food is causing a problem. This may be because taurine is such a classically known issue with cats that companies are much more “on-the-ball” in regard to taurine in cat food.
So that is it. I expect to hear from all of you in the next hour. Enjoy the end of summer. Be slightly less than all your energy demands.
Brett Grossman, DVM
Medical District Veterinary Clinic
Dr. Grossman’s Official Summer-Bummer Must-Read Cautionary Blog
Oh, it is the chronic role of a worrying veterinarian to introduce caution and concern into every joyous festivity.
- Little sister getting married? Why don’t you worry about your anxious cat at home not getting her proper medications while you left town?
- Moving into your new dream apartment? Did the previous tenants’ dog pass on his uncontrolled flea infestation to your little Boston terrier with skin issues?
- Tearing up the walls to finally build your new kitchen? I’d worry about fungal spores infecting your immunosuppressed cat who has been doing great on steroids for the last year.
This is such a classic role in the veterinarian’s party playbook that I feel very comfortable as your holiday mudpie summer-bummer storm cloud. Enjoy.
Chicago had collectively been wearing sweaters, hoodies, and winter coats from September to May. It is natural to now want to share the 90-degree weather with your animals as you bounce from outdoor festivals to block party to concerts and movies in the park to barbeques in the backyard to crowded bike and jogging paths, then to lake picnics, beer gardens, moderately overpriced sidewalk restaurants with faux-stone panels over bars stocked with Italian aperitivos named after lesser-known anarchist poets, the pool, and even just walks around the block.
I think when most people think of having a dog, this is what they imagine as the apex of the dog-human relationship. In theory, bringing our dogs (and cats, for some) with us is a wonderful idea, but there are some dangers about which you should be aware. Some are obvious, some are not.
Here are my tips/cautions/carefully worded and non-judgmental suggestions:
The Hot Hot Heat
If you are hot, imagine what your super bearded collie, or husky, or shaggy doodle is feeling.
You may think that a small jaunt to the corner store at noon will be a great time to get in a walk, but it may only take a short time away from water and coolness to send a dog into heat stroke. Bring a portable bowl, bring a bottle of water, find a cool place to go if you see signs of lethargy, heavy panting, weakness, vomiting, or abnormal behavior.
Don’t rely on community water bowls or on the kindness of shop owners to let you in the air-conditioned corner bakery, and don’t assume that clinical signs will get better while your pets rest on the sunny corner. Remember to cool your house in the afternoon for your animals, and really, at this point, does anybody need to tell you about the whole leaving-the-dog-in-the-car thing?
Chaos
Even the friendliest, most extroverted dogs may not like the sounds of marching bands, fireworks, the push of a crowd in their space, the smells of fire, and so on. Know your dogs’ fears and insecurities. Loud music, crowds, being cramped under a table, other dogs running around with and without leashes, strangers coming up to pet your dog … these scenarios can provoke unexpected responses, which can range from temporary to permanent trauma, lashing out and biting, anxiety-induced illnesses (colitis/diarrhea/vomiting), and, in some cases, really change your dog.
If you are the type who says things like, “I want to get my dog over his fear of air shows so I’m going to take him every year until he learns it’s a good thing,” then I’d like you to invite someone to force your greatest fears on you in an annual fashion. (Mine involve squids and Doritos and I do not want to talk about it.) If your dog does not seem right (too quiet, too scared, too excited), just take your Instagram photo to prove you were there and leave. Your dog will love you for it.
Dogs Everywhere
The exact place you thought of taking your super well-behaved dog is probably the same place that everyone else in the world thought of taking theirs too. Five individually well-behaved dogs does not necessarily make a well-behaved group of dogs.
Keep your dog away from others unless you receive a verbal cue from The Human that it is okay to have them mix, and even then, be careful. If you see signs of anxiety—some hackles raised, teeth bared under the smile—move on. Dog-fight wounds are one of the most common reasons we see animals on emergency.
Some establishments and public places do not want you to bring your dog with you, either for legal reasons or because they want to respect the non-dog people of earth. In places where dogs are allowed, there are plenty of kids and adults who see a dog and veer away. Don’t allow your dog to wander, even if on leash, and make others feel uncomfortable.
Leftover Food and Drinks
The aroma of hours-curdled cheese fries, vomit behind a beer stand, milkshake cups with cigarette butts, as well as the hot dog with onions in your hand, glasses of wine and beer laid to rest on the curbside graves of bar front, a Popeye’s chicken wrapper, a plate of brownies that may or may not also contain other substances in them, the wilted chocolate bar that melted on the picnic table, ETCETERA ETCETERA.
It doesn’t take much for your 10-pound dog to need therapy after ingesting some summertime waste and developing diarrhea, vomiting, and possibly pancreatitis. Just because you know what your dog ate doesn’t negate the need for therapy. If this happens, the sooner we treat, the easier it is to get through.
Absentee Owners
People steal dogs. Dogs get freaked out and run away. Just don’t leave them alone. Don’t go to stores that don’t allow dogs in them. Don’t go to a restaurant with your dog alone if you know you will need to go to the bathroom. I’m bored with this one.
Hotbeds of Disease
We all depend on the dog community to vaccinate their dogs to avoid transmitting disease and infections. Some vaccinations, such as rabies, are legally mandated, and others help provide herd immunity for dogs in Chicago.
We’ve had breakouts of leptospirosis, giardia, heartworm, canine influenza virus, and many other infectious diseases over the past few years despite these diseases being cheap and easy to vaccinate and protect against. If you think you are going to take your dog outside in the summer world, both respect the rest of the dog community by vaccinating and protecting your pet against fleas and ticks, and also respect your own dog, who is vulnerable. Most of these medications do not need a doctor’s exam by us to get as long as the pet has been seen in the last year.
The 4th of July
Most dogs hate fireworks. Help them through it. Anti-anxiety medications are effective, super cheap, relatively safe, and there is no reason to not help your pet through the storm of unexplainable and inconceivably frightening smashes of terror that, depending on the neighborhood, start in June and last for weeks after the Fourth.
If you are the type who thinks that anti-anxiety medications are for bad owners who can’t train their dogs’ fears away, or for cats who don’t feel safe in their home, we invite you to call and talk it over. It is not uncommon to have a slew of dogs and cats come in during early July with problems relating to their gastrointestinal system, urinary system, skin, eyes, etc., just due to the onslaught of subtle or obvious fear and anxiety.
Don’t bring your dogs out to see the fireworks. Give them a safe space at home that is muffled from the noise. You can see the AVMA’s tip guide here https://www.avma.org/public/PetCare/Pages/July-4-Safety.aspx
That is it. Avoid heat stroke. Read Spinoza.
Brett Grossman, DVM
Medical District Veterinary Clinic
Heartworm Disease: Why Your Pet Really Does Need Monthly Prevention
Heartworm disease, spread by mosquitoes, has been documented in all 50 states, and is considered endemic in 48 states. Both temperature and humidity play an important role in the life cycle of heartworms.
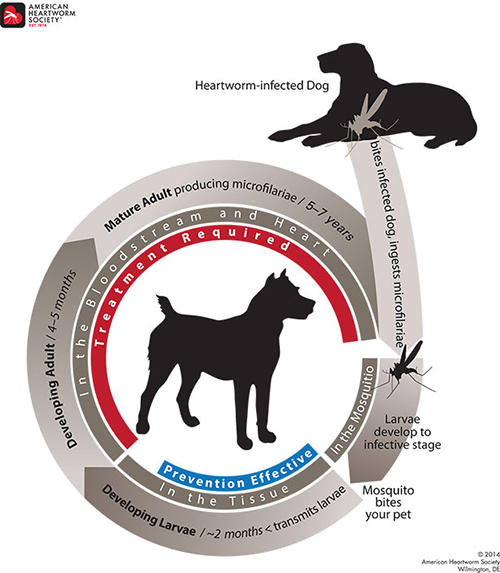
When a mosquito bites a heartworm-positive dog, the mosquito ingests the microfilaria (maggot stage of heartworm). Inside the mosquito, the microfilaria matures from a baby into a larva (little worm) and then injects the L3 larval stage back into dogs, infecting them with heartworms.
Below is a diagram of the life cycle of heartworms. Once infected, the worms can live five to seven years if they are never treated. You can also see that the monthly preventative is only effective at killing the developing larva (see blue “Prevention Effective” area). This is why it is so important to give prevention every month.
Watch a video of a heartworm case from one of our recent patients that shows microfilaria within the blood of a heartworm-positive dog.
Due to temperature and humidity playing an important role in the life cycle of heartworms, the transmission of heartworm disease is often limited to six to eight months in Chicago. For this reason, many people only give prevention during the “warm” months of the year. Only giving heartworm prevention during the “warm” months can place your dog at risk of developing this deadly disease. Below is an incidence map from the American Heartworm Society from 2016. As you can see, Chicago sees on average 26 to 50 cases/year per clinic.

How does heartworm prevention protect my dog?
When a dose of heartworm prevention is given to a dog (either topically or orally) it acts as a dewormer and kills off any of the possible larval stages that mosquitoes have transmitted to dogs. The medication is usually in and out of the dog’s system within 24 hours and does not stay in the dog’s body for 30 days. Heartworm prevention does not kill adult heartworms. It only kills the larval stages. This is why it is important to be given every 30 days because within 30 to 45 days post-exposure the larva can develop into juvenile adults, which the prevention is not effective at killing.
Why do I need to give prevention 12 months of the year, since the transmission of heartworm disease is limited to 6 to 8 months in Chicago?
There are two main reasons we recommend year-round prevention. First, there have been some studies that have shown that a single dose of heartworm prevention does not always kill off 100% of the larva, but repeated doses do kill 100%. Another reason monthly prevention is recommended is because most heartworm preventions also prevent intestinal parasites that can be spread to humans. Your dog can be exposed to these parasites by simply walking in areas where other animals (dogs or feral cats) defecate. When used monthly, your dog will also be dewormed against these parasites—roundworms and hookworms most commonly.
What if I miss a dose? Do I need to re-test before starting back on prevention?
If you miss a dose of prevention or are late giving it, just give it as soon as you remember. The annual heartworm test performed at annual wellness visits test for adult heartworms, and a single missed dose could lead to possible heartworms, but due to the life cycle it would take six to seven months for that test to show up positive. Therefore, we recommend if you miss a dose just start it back up as soon as possible and be sure to have your annual test completed within the next year to be sure that your dog did not get exposed to heartworms during the period in which he/she was unprotected.
Is heartworm disease considered contagious?
Not really. A dog can’t spread heartworms to another dog directly. A mosquito is always needed for transmission. With that in mind, having a heartworm-positive dog in the area does increase the risk for exposure as many mosquitoes may be infected with heartworm, waiting to transmit the disease to their next victim.
Drew Sullivan, DVM, Director
Medical District Veterinary Clinic
How to Ensure Your Pet Has the Longest, Healthiest Life Possible

May 6 through 12 is National Pet Week! This annual celebration sponsored by the American Veterinary Medical Association (AVMA) offers an opportunity for veterinarians to join with clients to promote responsible pet ownership and honor the many amazing pets in our lives.
This year’s theme is “Barks, Purrs, Tweets, Neighs … Pets Speak Love Many Ways.” (The above image shows the 2018 poster contest winner.)
Celebrating the special bond between people and pets reminds us of the importance of pet health care and the need for owners and veterinary caregivers to partner to keep four-legged family members as healthy and happy as possible.
To celebrate the 35th anniversary of National Pet Week, AVMA has shared seven specific values that every pet owner should consider to ensure that their pet lives the longest, healthiest life possible.
1. Choose well, commit for life
Select the pet that’s right for your family’s lifestyle and make a commitment to that pet for its life. Even if you have already welcomed a pet into your home, your veterinarian can help you better understand the social and health care needs of your individual pet.
2. Socialize now—new doesn’t have to be scary
Learn about how to appropriately prepare your pet to enjoy a variety of interactions with other animals, people, places and activities. Everyone will be more comfortable!
3. Nutrition and exercise matter
With an estimated 53% of dogs and 58% of cats in the United States considered overweight or obese, and humans plagued by this issue as well, the AVMA encourages pets and their owners to get proper nutrition and regular exercise—together! This not only improves cardiovascular health, maintains a healthy weight, and supports good mental health for both owner and pet, but it also strengthens the human-animal bond. For tips on walking, running, or starting another exercise program with your pet, visit avma.org/Walking. Visit avma.org/nutrition for more information on your pet’s healthy weight.
Step It Up! is the Surgeon General’s initiative to promote walking. The program encourages brisk walking to reduce the risk of heart disease and diabetes in people. Dog owners know there is no better motivator for a walk than their canine companion. Recent scientific studies show that dog owners may get more exercise and are less likely to be obese than those who don’t own or walk a dog. Owners that walk their dog also had greater mobility within their homes. Other studies have shown that all pets, not just dogs, have been shown to lower heart rates and blood pressure as well as promote quicker recovery times from stressful events.
The Centers for Disease Control recognizes that keeping pets healthy keeps people healthy too. Visit cdc.gov/healthypets for more information.
4. Love your pet? See your vet!
Everybody loves their pet, yet a majority of cat owners and nearly half of dog owners do not take their pet to the veterinarian unless it is visibly sick or injured. Pets often hide signs of illness. Reular check-ups are vital to catching health problems early. Early treatment means better health for your pet. It can also save money!
5. Pet population control: Know your role
Do your part to prevent pet overpopulation. Talk to your veterinarian about when you should have your pet spayed or neutered. Avoid unplanned breeding through spay/neuter, containment, or managed breeding. To learn more, visit the AVMA webpage on spaying and neutering your pet.
6. Emergencies happen. Be prepared.
Include your pets in your family’s emergency plan. The AVMA offers a step-by-step guide to assembling emergency kits and plans for a variety of pets and animals.
7. Give them a lifetime of love
Thanks to better care, pets are living longer now than they ever have before—but as pets get older, they need extra care and attention. Regular veterinary examinations can detect problems in older pets before they become advanced or life-threatening, and improve the chances of a longer and healthier life for your pet.
Visit the AVMA’s special page for senior pets to find out what is “normal” and what may signal a reason for concern about an aging pet. Contrary to popular belief, dogs do not age at a rate of seven human years for each year in dog years.
To honor and celebrate all of the amazing dogs and cats that are a part of our Medical District Veterinary Clinic family, we invite you to bring in your favorite pictures, so we can post them around the clinic. You can also email them to gethelp@medicaldistrictvet.com. We can’t wait to see all of the adorable photos!
Amber Slaughter, DVM
Medical District Veterinary Clinic
Putting the ‘Anal Sac’ in ‘Banal Sacrifices’

Most of us in the veterinary field face a horrible dilemma. The majority of our days are filled with details and particulars that are deemed rather unfit for discussion at the dinner table, any social gathering, and anywhere outside the professional confines of the clinic. It’s always fun to talk puppies and kittens, but a great deal of what we do during the day revolve around bodily fluids (blood, feces, urine, vomit), wounds, parasites, and the selected greatest and grossest hits of infection and disease.
Anything interesting happen at work today? Yes. Most of it was gross.
So, I’d like to discuss the grossest of all things for one moment. Please feel free to put away your chocolate custard, beef stew, and bean soup, for one moment, while we explore dog and cat anal sac disease.
Cats and dogs have anal sacs located near the periphery of the anus. These sacs excrete a liquid, often when animals defecate, that mixes into their stool and gives forth a particular and specific smell akin to a garbage bag filled with a rotting animal that has been soaked in plague juice. At times, though, the ducts that excrete the anal sac fluid can become blocked, forcing the sacs to become enlarged, uncomfortable, swollen, and irritated. Sometimes these sacs can become so blocked that they burst forth with a mixture of all of the aforementioned dinner-party unmentionables in one fell swoop. Other times they slowly leak out at convenient times and places such as Sunday morning at 5:13 a.m. on your pillow next to your head. Often, they don’t do anything but get bigger and more uncomfortable. There are times when severe stress and discomfort can cause animals to release their anal sacs all over (seemingly) everywhere in the world.
Owners complain about their dogs and cats “scooting” their back ends over the ground or that their pets are licking their back end obsessively. The clinical signs may be more vague and scary, especially for older animals who have not ever had this problem. We may find out animals straining to defecate (as the sacs block the exit of the anus), walking stiffly, uncomfortable, not interested in eating, and, in extreme cases, vomiting. I’ve seen some dogs become so affected that they scream in pain when touched and refuse to move. I’ve seen some cats stop eating or moving and refuse to go into the litter box.
Why does this happen? you ask (while not at the dinner table). There are a few common reasons:
• Anatomical irregularities that are uncontrollable: Some dogs and cats, for whatever reason, just don’t seem to have anal sacs or anal sac ducts in the right position to allow for easy release. We have seen puppies whose anal sacs fill up monthly and need help.
• An extended period when the animal’s feces are soft and unable to naturally press on the sacs to express them: When animals have parasites (such as Giardia) or chronic diarrhea due to dietary issues or underlying illnesses, we often are not thinking that during the whole of this period, their anal sacs are (metaphorically) laughing with power as they grow bigger.
• Infiltrative disease (such as cancer): This is not very common, though it can occur. The anal sacs become diseased and cancerous. It can happen in any dog, but one tends to see this more in spaniel breeds. It does not have a good prognosis, but this condition is rare. Very rare.
• Animals, especially as they get older, learn different postures to deal with changes in the body. I have seen so many cats and dogs with untreated back pain that have to posture differently to defecate, and because of this, do not seem to express their anal sacs with the same proud efficiency that they once did. As the anal sacs get worse, they become even more uncomfortable, the animals defecate less, develop chronic soft stool, and this glorious cycle continues until you have a cat or dog that is constipated and has horribly painful anal sacs.
What can you do about it?
First, express the anal sacs. This is not something one should just try at home. I am speaking for all citizens of earth, in general, by saying that you should not do this in your kitchen before the family wakes up. Partly, because the smells of putrid sub-par day-old fish byproduct mixed with armpits and feces will probably wake them up, but also I wonder if this aspect of your relationship with your pet is one you really want to explore. While some people do learn to do this at home with their animals, I personally will not do it at home on my animals. But it is possible.
Alternatively, we can express your animal’s anal sacs so you don’t have to watch, smell, see, and, in some tragic cases, taste. We have safe zones in the clinic where no one walks for fear of spraying anal sacs. Some groomers do this for you, but few do them to completion. Ask your groomer before you assume, and talk with us about how soon you should come back for a recheck. Sometimes the anal sacs can be so full and painful that sedation may be required.
Second, animals may need additional treatment, such as antibiotics or anti-inflammatories. Most bad cases of anal sacculits, anal sac impaction, or anal sac abscesses need medication and aggressive rechecks before they are not painful or affected. It’s not generally the case that medications alone will work.
Third, we must remove the cause. Are allergies causing chronic licking, which is causing the anal sacs to be inflamed? Is your animal’s diet not allowing for a normal stool texture? Do you need to add fiber to the diet? Is your dog anxious, and this anxiety manifests in back-end licking? Are there intestinal parasites present? Is there infiltrative disease? Is there a chronic infection? Is there another animal in the house that is over-grooming the affected animal? We need to fix this.
Fourth, sometimes the anal sacs need to be removed. It’s not a cheap therapy, and it is surgery. But sometimes after coming into the clinic every two weeks and having anal sac disease a constant part of their lives, some owners elect to remove them.
As a final note, most dog owners know or have heard of anal sac issues, but most cat people are thinking that this is not applicable. This problem affects many mammals. So I’m sorry to say that even the sweetest of felines has the foulest of anal sac scents. I’ve had a run, lately, of seemingly ill cats who magically became “new” cats after their anal sacs were expressed. And, for those who play with the skunks, beavers, and opossums of your neighborhood, though I’m sure you have more on your mind, also be aware. Humans have them too, but I will let you and your loved ones google that on your own on your non-work computer.
Enjoy the warm weather. It will make things more convenient for when you need to open the windows after the scent of your animal’s anal sacs permeate the walls of your Chicago apartment.
Brett Grossman, DVM
Medical District Veterinary Clinic
FAQs on Pet Insurance

Have you considered purchasing pet insurance? Or do you already have pet insurance? More and more pet owners are purchasing insurance, but still, only a very small percentage of pet owners have it. I hope I can answer some of the common questions I receive from clients regarding pet insurance.
Why do I need pet insurance?
In veterinary medicine we use many of the same diagnostics, medications, and therapies used in human medicine and as everyone knows, going to the doctor is very expensive. Unfortunately, many treatment decisions for pets are determined by the cost associated. If an owner has pet insurance, cost does not become the determining fact. Cost still needs to be factored in, but an owner can focus on the pet’s condition and the possible treatment options and decide what is best for the pet.
When is the best time to sign up?
Since insurance companies do not cover pre-existing conditions, it is best to sign up as soon as you get your dog or cat. Too often owners wait when their pet requires intensive medical treatments, and then wish they had signed up sooner.
What is covered in my insurance plan?
Every insurance plan is different and every company has different coverage plans. It is very important that you do your research and know what your plan covers. In most cases, pet insurance covers accident and illness, but does not cover wellness care. There are a few insurance companies that offer full coverage (meaning wellness care is covered), but these monthly premiums are typically a lot more expensive. Additionally, based on your pet’s medical history, certain conditions may be considered pre-existing conditions and not be covered. I always recommend looking at the part of your plan that highlights what is NOT covered, as this is likely easier to understand compared to what is covered.
How is this different from human insurance?
One of the biggest differences between pet insurance and human insurance is the fact that, with pet insurance, owners must pay up front, and then the insurance company reviews the owner’s claim and reimburses the owner. In veterinary medicine, the veterinarian does not handle insurance claims as is done in human medicine. Pet owners must have the means to pay for all services up front, then apply for reimbursement from the insurance company. This is another differentiating feature of insurance companies that pet owners should consider. I recommend looking at the average turnaround time from when a claim is submitted until the reimbursement is complete.
What insurance company do you recommend?
There are many insurance companies on the market, and I feel there are many good options. It really comes down to what your goal is with insurance. Things to consider:
- What is the monthly premium?
- What is the deductible? Is it an annual deductible or per incident?
- What is the coverage? (Usually 70%, 80%, 90%, or 100%)
- Is there an annual limit? Per incident limit? Or lifetime limit on the policy?
- What is NOT covered in the policy?
- How quick does the company provide reimbursement?
Drew Sullivan, DVM, Director
Medical District Veterinary Clinic

![[lost pet flier]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2019/08/mdvc-lost-pet.jpg)
![[doberman pinscher]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2019/07/blog-grossman-dcm2.jpg)
![[wall graffiti of red monster]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2019/05/blog-fear-graffiti.jpg)


