Posts in Category: The Cat’s Meow
Urinary Changes in Your Pets

It is always an unhappy surprise when we find a spot of urine somewhere other than the litter box or a potty pad. Especially when it’s on your pile of clothes.
Knowing your pet’s normal urine schedule can be a great help for getting to the bottom of episodes that are outside their routine. Urine changes in a cat or a dog can be caused by very mild to very severe and potentially fatal medical conditions, so it is important to address any changes quickly.
This blog addresses various health conditions that can lead to urinary changes in cats and dogs. You’ll learn clinical signs to watch for, diagnostic tests performed to help determine the cause of these changes, possible medical or surgical treatment options, and what to expect long term.
Urinary Tract Infection (UTI)
The urinary tract consists of the kidneys, the bladder, and the ureters (which carry urine from the kidneys to the bladder). Although a dog or cat can get an infection in any of these three regions, bladder infections are the most common.
Clinical signs may include polyuria, which means frequent urine episodes, such as going in and out of the litter box, or having multiple small streams of urine instead of one large stream. Other clinical signs range from blood in the urine, pain or discomfort when urinating, and posturing to urinate with no urine being produced to odorous urine or lethargy, indicating your pet is not feeling well or is uncomfortable.
An easy inexpensive diagnostic test that can be performed to rule in/out a UTI is a urinalysis. This is a great screening test that allows us to assess the urine for pH changes, specific gravity, crystals, bacteria, white blood cells, etc.
Although a free-catch sample (a sample collected at home) is great, a cystocentesis can be performed in the clinic to obtain a sterile sample. After an ultrasound is used to find the bladder, a sterile needle is inserted to obtain a sample externally. If bacteria are present, the patient has a UTI.
Once a UTI is confirmed, the next step is a urine culture, which means that the laboratory will grow the bacteria in the urine and let us know what antibiotic will treat the infection. Follow-up rechecks with your veterinarian are important to assure that the infection is cleared, as bacteria can become resistant to antibiotics.
Once the infection is gone, the pet’s prognosis is good. Patients with recurrent UTIs may need a long-term prescription urinary diet to keep their pH at a level that does not allow bacteria to grow. This diet will help prevent new infections.
Bladder Stones and Crystals
Stones start off as crystals in the bladder. Crystals may arise due to a variety of factors, such as pH changes and increased urine concentration. Bladder stones come in many types, including struvite, calcium oxalate, urate, cysteine, xanthine, and calcium phosphate.
Fun Facts
- What are the two most common types of bladder stones?
Struvite and Calcium Oxalate - What type of bladder stone is commonly associated with urinary tract infections?
Struvite - Which bladder stone is hormonally dependent and more common in a male dog that has not been neutered?
Cysteine - Why are Dalmatians predisposed to urate stones? (Urate stones are a type of kidney stone formed when uric acid crystals accumulate in the urinary tract.)
Dalmatians have a gene mutation that interferes with uric acid metabolism, causing high levels of uric acid in the body, which concentrates in the urine and leads to stones.
Clinical signs of bladder stones include straining to urinate, dribbling urine, blood in the urine, and pain/discomfort when urinating. Bladder stones can be diagnosed via ultrasound of the bladder and abdominal radiographs. If large enough, they can even be palpated manually. Keep in mind that certain types of bladder stones are not visible on radiographs, so it is important to assess the patient as a whole.
It is always important to check a urine sample to look for an infection. Struvite stones are commonly associated with UTIs. Once the UTI is cleared, then the stone can dissolve.
If a UTI is not present or if a UTI is cleared and a stone remains, then the next step is a prescription urinary diet. The goal of the prescription diet is to change the pH of the urine to allow the stone to dissolve and prevent new stone formation. Some patients may not need to be on a prescription urinary diet long term, however, most patients will.
If the patient is on a urinary diet and the stone is not dissolving or getting smaller, then the next step is surgery. A cystotomy is a surgical procedure performed to remove the stone from the patient’s bladder. Left untreated, stones can become large enough to make urination difficult, which can lead to blockage and life-threatening situations.
Your pet should be urinating daily. A blocked cat or dog is a medical emergency.
Kidney Disease
The kidneys help produce urine and remove toxins from the body. They also help manage hydration, blood pressure, production of red blood cells, and calcium/ phosphorus balance.
The filtration unit of the kidney is called a nephron. As a patient ages, so do the nephrons. If kidney tissue ceases to do its job of filtration, normal function cannot be maintained.
Clinical signs of kidney disease include polyuria (increased frequency of urination), polydipsia (increased water intake), decreased appetite, vomiting, and lethargy in advanced cases.
Kidney disease is diagnosed via blood screening tests along with clinical signs. Kidney disease is irreversible. Treatment depends on the stage and severity of kidney disease. The patent will likely need to be on a prescription kidney diet long term. It is important to check blood pressure, as many patients will have to be on additional medications. If left untreated, kidney disease can be fatal.
Endocrine Conditions
A few conditions related to hormones result in urinary changes in pets.
Hypothyroidism results from decreased thyroid hormone production by the thyroid gland. This condition is more common in dogs than in cats. Clinical signs include weight gain, polyuria, polydipsia, and fatigue.
Hyperthyroidism, on the other hand, is an overproduction of thyroid and is more common in cats. Clinical signs include weight loss, ravenous appetite, polyuria, and polydipsia.
Hypo/hyperthyroidism can be diagnosed via routine blood work and are both medically managed.
Diabetes mellitus is caused by a deficiency in insulin, which is produced by the pancreas. Diabetes can be diagnosed via routine blood work, a fructosamine, along with clinical signs. Clinical signs include polyuria, polydipsia, and weight loss.
With elevated glucose levels in the bloodstream, glucose can spill into the urine in high amounts. Glucose in the urine can lead to bacteria growth leading to urinary tract infections, which are common findings in diabetic patients.
Treatment for diabetes entails daily subcutaneous insulin injections.
Bladder Tumors
Bladder tumors, unfortunately, display similar signs to both urinary tract infections and bladder stones. These include straining to urinate, dribbling urine, blood in the urine, pain/discomfort when urinating, and abdominal pain/discomfort.
A bladder tumor may be suspected if, during a cystocentesis, the ultrasound indicates an abnormality in the bladder. If large enough, bladder tumors can also be seen on radiographs.
Treatment of a bladder tumor depends on the type of tumor and will be determined by working with a veterinary oncologist.
As you can see, urinary changes can range from mild to severe. As veterinarians, our job is to investigate the underlying cause of your pet’s health changes. If you notice any urinary changes in your pet, please see your local veterinarian.
— Dr. Angélica Calderón
Cambios de Orina en Sus Mascotas

Siempre es una gran sorpresa cuando encontramos una mancha de orina de nuestra mascota en algún lugar que no sea apropiado.
Conocer el horario normal de micción de tu mascota puede ser una gran herramienta para lidiar con cualquier episodio que se salga de su rutina habitual. Los cambios en la orina de un gato o un perro pueden ser causados por condiciones médicas desde muy leves hasta muy graves y potencialmente fatales, por eso es importante visitar a su veterinario cuando note cambios de orina en sus mascotas.
Discutiremos varias condiciones de salud que pueden provocar cambios urinarios en gatos y perros y sus signos clínicos a monitorear, pruebas de diagnóstico realizadas para ayudar a determinar la causa de los cambios, opciones médicas o quirúrgicas (si es necesario), mantenimiento y pronóstico.
Infección del Tracto Urinario
El tracto urinario está formado por los riñones, los uréteres y la vejiga. Aunque un perro o un gato pueden contraer una infección en cualquiera de estas tres regiones, las infecciones de la vejiga son las más comunes. Algunos signos clínicos incluyen poliuria (episodios frecuentes de orina), como entrar y salir de la caja de arena o tener múltiples chorros pequeños de orina en lugar de un chorro grande. Otros signos clínicos incluyen sangre en la orina, dolor o malestar al orinar, posturas para orinar sin producir orina, orina con olor y letargo si su mascota no se siente bien o está incómoda.
Una prueba de diagnóstico sencilla y económica que se puede hacer para descartar una infección urinaria es un análisis de orina. Esto nos permite evaluar la orina en busca de cambios de pH, gravedad específica, cristales, bacterias, glóbulos blancos, etc. Aunque una muestra de orina recogida en casa es una buena opción, se puede hacer una cistocentesis en la clínica para obtener una muestra estéril. Esto se realiza mediante el uso de un ultrasonido para encontrar la vejiga; luego se utiliza una aguja estéril para obtener una muestra externa. Si hay bacterias, se confirma la presencia de una infección urinaria en el paciente. Una vez confirmada la infección urinaria, el siguiente paso es un cultivo de orina, lo que significa que el laboratorio hará crecer las bacterias en la orina y nos informará qué antibiótico tratará la infección. Los controles de seguimiento con su veterinario son importantes para asumir que la infección se ha curado, ya que las bacterias pueden volverse resistentes a los antibióticos.
Algunos pacientes con infecciones urinarias recurrentes necesitarán una dieta urinaria prescrita a largo plazo para mantener el pH en un nivel que no permita el crecimiento de bacterias, lo que ayudará a prevenir nuevas infecciones. Una vez que la infección haya desaparecido, el pronóstico es bueno.
Cálculos y Cristales en la Vejiga
Los cálculos comienzan como cristales en la vejiga y pueden deberse a diversos factores, como cambios de pH y aumento de la concentración de orina. Existen muchos tipos de cálculos en la vejiga, como los de estruvita, oxalato de calcio, urato, cisteína, xantina, fosfato de calcio, etc.
Datos curiosos
- Cuáles son los dos tipos más comunes de cálculos en la vejiga?
Estruvita y oxalato de calcio - Qué tipo de cálculo en la vejiga se asocia comúnmente con infecciones del tracto urinario?
Estruvita - Qué cálculo en la vejiga depende de las hormonas y es más común en un perro macho intacto?
Cisteína - Por qué los dálmatas están predispuestos a los cálculos de urato?
Los dálmatas tienen una mutación genética que interfiere con el metabolismo del ácido úrico y causa altos niveles de ácido úrico en el cuerpo, que se concentra en la orina y produce cálculos.
Los signos clínicos incluyen esfuerzo para orinar, goteo de orina, sangre en la orina, dolor o malestar al orinar, etc. Los cálculos en la vejiga se pueden diagnosticar con ultrasonido de la vejiga y radiografías abdominales; si son lo suficientemente grandes, incluso se pueden palpar manualmente si están grandes. Hay ciertos tipos de cálculos en la vejiga que no son visibles en las radiografías, por lo que es importante evaluar a todo el paciente.
Siempre es importante analizar una muestra de orina para evaluar si hay una infección, ya que los cálculos de estruvita se asocian comúnmente con las infecciones urinarias. Una vez que se cura la infección urinaria, el cálculo puede disolverse. Si no hay una infección urinaria o si se cura y queda un cálculo, el siguiente paso es una dieta urinaria recetada. El objetivo de la dieta recetada es cambiar el pH de la orina para permitir que el cálculo se disuelva y evitar la formación de nuevos cálculos. Depende de cada paciente si necesitará seguir una dieta urinaria recetada a largo plazo, pero la mayoría de los pacientes lo harán. Si el paciente sigue una dieta urinaria y el cálculo no se disuelve o no se hace más pequeño, el siguiente paso es la cirugía. Una cistotomía es un procedimiento quirúrgico que se realiza para extraer el cálculo de la vejiga del paciente. Si no se trata, los cálculos pueden llegar a ser lo suficientemente grandes como para dificultar la micción, lo que puede provocar un bloqueo y situaciones potencialmente mortales. Su mascota debe orinar a diario. Un gato o perro bloqueado es una emergencia médica.
Enfermedad Renal
Los riñones ayudan a producir orina y a eliminar toxinas del cuerpo. También ayudan a controlar la hidratación, la presión arterial, la producción de glóbulos rojos y el equilibrio calcio/fósforo. La unidad de filtración del riñón se llama nefrona. Cuando una mascota envejece, las nefronas también envejecen. Sin tejido renal funcional no se puede mantener una función normal. Los signos clínicos de la enfermedad renal incluyen poliuria (aumento de la frecuencia de micción), polidipsia (aumento de la ingesta de agua), disminución del apetito, vómitos y letargo si está avanzado.
La enfermedad renal se diagnostica por análisis de sangre y signos clínicos. La enfermedad renal es irreversible y el tratamiento depende de la etapa de la enfermedad y de lo avanzada que esté. Es probable que el paciente deba seguir una dieta renal recetada a largo plazo. Es importante controlar la presión arterial, ya que muchos pacientes deberán tomar medicamentos adicionales. Si no se trata, la enfermedad renal puede ser mortal.
Condiciones de Endocrinas
El hipotiroidismo es el resultado de una disminución de la producción de hormona tiroidea por parte de la glándula tiroides, más común en los perros. Los signos clínicos incluyen aumento de peso, poliuria, polidipsia y fatiga. Por el contrario, el hipertiroidismo es más común en los gatos y es la sobreproducción de hormonas. Los signos clínicos incluyen pérdida de peso, apetito voraz, poliuria y polidipsia. El hipotiroidismo y el hipertiroidismo se pueden diagnosticar mediante análisis de sangre de rutina y ambos se tratan con medicamentos. Como puede ver, estas afecciones también implican cambios urinarios en una mascota.
La diabetes mellitus es causada por una deficiencia de insulina, que es producida por el páncreas. La diabetes se puede diagnosticar mediante análisis de sangre de rutina, una fructosamina, junto con los signos clínicos. Últimamente, el tratamiento implica inyecciones subcutáneas diarias de insulina. Los signos clínicos incluyen poliuria (micción excesiva), polidipsia (ingesta excesiva de agua) y pérdida de peso. Con niveles elevados de glucosa en el orine, la glucosa puede derramarse en la orina en grandes cantidades. La glucosa en la orina puede provocar el crecimiento de bacterias que provocan infecciones del tracto urinario, que son hallazgos comunes en pacientes diabéticos.
Tumores de Vejiga
Los tumores de vejiga pueden presentar síntomas similares a las infecciones del tracto urinario y a los cálculos vesicales, como esfuerzo para orinar, goteo de orina, sangre en la orina, dolor o malestar al orinar y dolor o malestar abdominal. Se puede sospechar un tumor de vejiga si se observa una anomalía en ultrasonido mientras se examina la vejiga durante una cistocentesis. Si son lo suficientemente grandes, los tumores de vejiga también se pueden ver en las radiografías. Una vez que se diagnostica un tumor de vejiga, el tratamiento se basa en el tipo de tumor. Aquí es donde el dueño de la mascota trabajará junto con un oncólogo veterinario para determinar el mejor plan de tratamiento para su mascota.
Como puede ver, los cambios urinarios pueden variar de leves a graves y nuestro trabajo como veterinario es investigar la causa subyacente de los cambios en la salud de su mascota. Si nota algún cambio urinario en su mascota, consulte a su veterinario local.
— Dr. Angélica Calderón
New Year’s Resolution: No Overweight Pets

With the start of the new year, you might have noticed an increase in the number of gym memberships and more people waiting in line to use the elliptical. If you’ve also noticed that your pet at home has packed on a couple of extra holiday pounds, now would be a perfect time to start considering some weight loss for your pet. Increased weight can lead to obesity, and various negative health conditions can follow.
How Do I Know If My Pet Is Overweight?
Pets are given a body condition score (BCS) to determine if they are overweight, underweight, or at an ideal body weight. BCS is determined not only by the number on the scale and physical appearance, but also fat deposits felt by your veterinarian during the exam along with amount of muscle mass. Below are charts from the Association for Pet Obesity Prevention that illustrate body condition scores for dogs and cats. Please reach out to your local veterinarian if you would like to know if your pet is overweight.
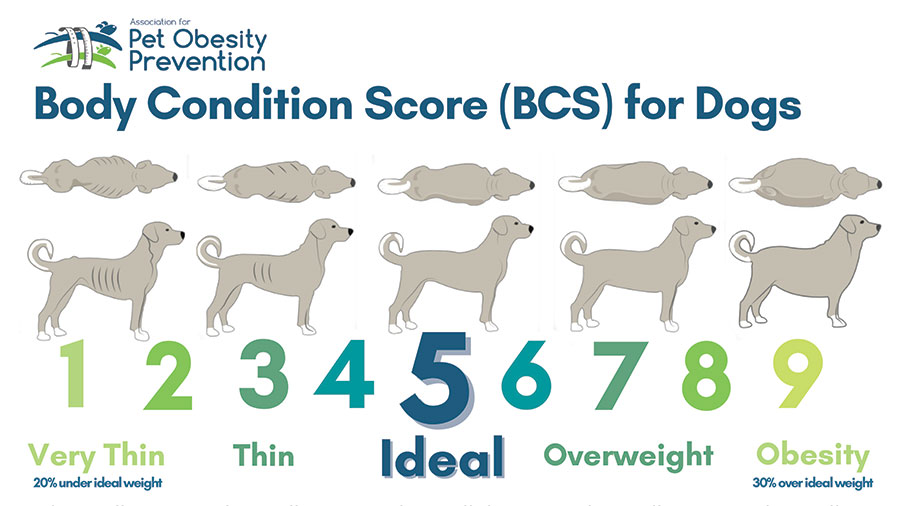
- Ribs visible from a distance under shorthair, no palpable body fat
- Ribs visible under shorthair, no palpable fat
- Ribs may be visible under shorthair, no palpable fat
- Ribs minimally visible, easy to palpate with minimal fat cover
- Ribs not visible, easy to palpate with minimal fat covering
- Ribs palpable under mild fat covering
- Ribs palpable with difficulty under moderate fat covering. Mild fat deposits over lumbar area and tail base
- Ribs palpable only with significant pressure under marked fat deposits. Moderate fat deposits over lumbar area and tail base
- Ribs not palpable under marked fat deposits. Marked fat deposit over spine including the neck and tail base
What Are the Health Risks?
Obesity is associated with many negative health conditions. Such conditions include joint disease and osteoarthritis, heart disease, respiratory distress, decreased grooming in cats, diabetes mellitus, increased anesthetic risk, and ultimately a decreased lifespan.
Joint Disease and Osteoarthritis: Extra weight adds extra pressure and stress on joints, which can lead to early joint degeneration and decreased mobility. This, in turn, can exacerbate obesity. In a patient undergoing a weight loss journey, adding joint supplements can help strengthen joints, which may increase mobility and comfort, ultimately helping with weight loss.
Diabetes Mellitus: Extra body fat can lead to insulin resistance. Weight loss can help decrease a cat’s risk for the development of diabetes mellitus. According to a study at Cornell University College of Veterinary Medicine, obese cats are four times more likely to develop diabetes than are cats with an ideal BCS.
Heart Disease: Although fat is relatively nonvascular tissue, it still requires blood flow, which leads to an increase in circulatory volume and cardiac output, ultimately resulting in hypertension. Compared to dogs with an ideal body weight, obese dogs develop negative changes to the overall structure and function of their heart.
Why Do Pets Become Overweight?
Well, we are the culprits. Overfeeding, lack of exercise, and too many treats can lead to obesity in pets. Various endocrine diseases are associated with obesity, such as Cushing’s disease and hypOthyroidism in dogs. In cats, weight loss and low BCS are commonly associated with hypERthyroidism.
What Do I Do If My Pet Is Overweight?
Weight loss can be a hard, slow process. It takes much time and patience. When your veterinary team works with you and provides the right tools, we can achieve a healthy weight for your pet.
There are many dietary changes that can be done in order to achieve weight loss in your pet. A great start is checking out the Pet Nutrition Alliance website. When you enter your dog’s current weight and body condition score, this website calculates a calorie count for you. It is important to account for all food AND treats using this calorie count. Please reach out to your local veterinarian if you would like to know your pets BCS.
There are several over-the-counter options as well as prescription diets that can be given to your pet for weight loss. When feeding in cups, it is important to use an actual measuring cup to avoid overfeeding/underfeeding. Calories per cup can vary, so please check the back of the bag for an accurate calorie measurement of how many cups your pet should be eating. Healthy, low-calorie fruits and vegetables such as apple slices, carrots, celery, and cucumber can be used as treats. Please avoid grapes, raisins, onion, garlic, and avocados, which can be highly toxic to pets.
Exercise is a very important component in order to achieve weight loss. Therefore, adding more play time, frequent walks, and possibly even a kitty treadmill can help achieve your pet’s weight loss goals. Frequent weigh-ins are also a very important component for weight loss to track the progression of your pet’s weight.
If you suspect that your pet is overweight, please reach out to your primary care veterinarian to you can discuss the best option for your pet.
From ‘Fat Vincent’ to ‘Skinny Vinny’
In 2016, a 7-year-old obese dachshund named Vincent was surrendered to an animal shelter in Houston, Texas, after his owner died. He weighed 38 pounds. Thanks to the help of K-9 Angels Rescue, he was able to lose over half of his body weight and was renamed Skinny Vinny. He weighed in at 17 pounds after an 8-month weight-loss journey.
By Dr. Angélica Calderón
Dog image: VinnieRattolle, CC BY-SA 4.0, via Wikimedia Commons
Propósitos de Año Nuevo para todos
Con el comienzo del nuevo año, es posible que hayas notado un aumento en el número de membresías en gimnasios y más personas esperando en fila para usar la máquina elíptica. Ahora, si ha notado que su mascota en casa subio un par de kilos de más durante las vacaciones, entonces sería un momento perfecto para comenzar a considerar perder algo de peso; ya que el aumento de peso puede provocar obesidad y pueden producirse diversas condiciones negativas de salud.
¿Cómo puedo saber si mi mascota tiene sobrepeso?
A las mascotas se les asigna una puntuación de condición corporal (también conocida como BCS) para determinar si tienen sobrepeso, bajo peso o si tienen un peso corporal ideal. Comuníquese con su veterinario local si desea saber si su mascota tiene sobrepeso.
A continuación se muestran gráficos de la Asociación para la Prevención de la Obesidad de las Mascotas que ilustran las puntuaciones de condición corporal de perros y gatos. Comuníquese con su veterinario local si desea saber si su mascota tiene sobrepeso.
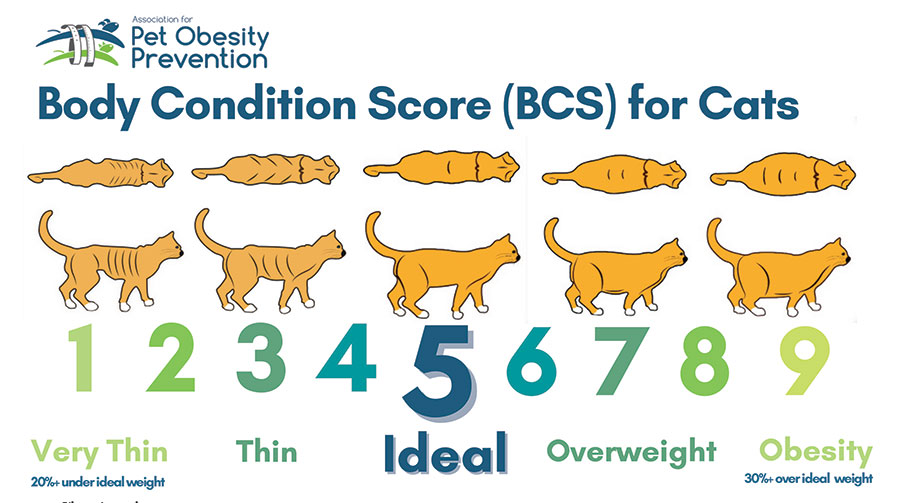
- Costillas visibles desde lejos debajo del pelo corto, sin grasa corporal palpable
- Costillas visibles debajo del pelo corto, sin grasa palpable
- Las costillas pueden ser visibles debajo del pelo corto, no se palpa grasa
- Costillas mínimamente visibles, fáciles de palpar con mínima cobertura de grasa
- Costillas no visibles, fáciles de palpar con una cobertura mínima de grasa
- Costillas palpables bajo una leve capa de grasa
- Costillas palpables con dificultad bajo una cubierta grasa moderada. Depósitos leves de grasa sobre la zona lumbar y la base de la cola.
- Costillas palpables sólo con una presión significativa bajo depósitos de grasa marcados. Depósitos moderados de grasa sobre la zona lumbar y la base de la cola.
- Costillas no palpables bajo depósitos de grasa marcados. Depósito de grasa marcado sobre la columna, incluido el cuello y la base de la cola.
¿Cuales son los riesgos para la salud?
La obesidad está asociada con muchas condiciones de salud negativas. Dichas afecciones incluyen enfermedades como osteoartritis, enfermedades cardíacas, dificultad respiratoria, disminución del aseo en los gatos, diabetes mellitus, mayor riesgo anestésico, y en casos graves menos tiempo de vida.
Enfermedades de osteoartritis: El peso extra añade presión y estrés adicionales a las articulaciones, lo que puede provocar una degeneración temprana de los huesos y una disminución de la movilidad, lo que a su vez puede exacerbar la obesidad. En un paciente que está pasando por un proceso de pérdida de peso, agregar suplementos para los huesos puede ayudar a fortalecer los huesos, lo que puede conducir a una mayor movilidad y mayor comodidad.
Diabetes mellitus: El exceso de grasa corporal puede provocar resistencia a la insulina y la pérdida de peso puede ayudar a disminuir el riesgo de que un gato desarrolle diabetes mellitus. Según un estudio de la Facultad de Medicina Veterinaria de la Universidad de Cornell, los gatos obesos tienen cuatro veces más probabilidades de desarrollar diabetes que un gato con un BCS ideal.
Enfermedad cardíaca: Aunque la grasa es un tejido relativamente no vascular, aún requiere perfusión, lo que conduce a un aumento en el volumen circulatorio y el gasto cardíaco, lo que puede resultar en hipertensión. En comparación con los perros con un peso ideal, los perros obesos tienen varios cambios en la estructura y función general de su corazón.
¿Por qué las mascotas tienen sobrepeso?
Bueno, nosotros somos los culpables. La sobrealimentación, la falta de ejercicio y demasiados premios pueden provocar obesidad en las mascotas. Varias enfermedades endocrinas están asociadas con la obesidad, como la enfermedad de Cushing y el hipotiroidismo en perros, mientras que la pérdida de peso y un nivel bajo de BCS pueden estar asociados con el hipertiroidismo en los gatos.
¿Qué hago si mi mascota tiene sobrepeso?
La pérdida de peso puede ser un proceso lento y difícil y requiere mucho tiempo y paciencia. Somos un equipo pero con las herramientas adecuadas podemos lograr un peso saludable para tu mascota.
Hay muchos cambios en la dieta que se pueden realizar para lograr la pérdida de peso de su mascota. Un buen comienzo es visitar el sitio web de Pet Nutrition Alliance. Este sitio web le permite ingresar el peso actual de su perro junto con su puntuación de condiciones corporales. Se calcula un recuento de calorías. Es importante tener en cuenta todos los alimentos y premios utilizando este recuento de calorías.
Hay varias opciones de venta libre, así como dietas recetadas que se pueden administrar a su mascota para bajar de peso. Varias marcas de alimentos de venta libre tienen una fórmula “baja en calorías” o de “peso perfecto”. Al alimentar en tazas, es importante utilizar una taza medidora para evitar la sobrealimentación o la subalimentación. Las calorías por taza varían, así que revise la parte posterior de la bolsa de comida para obtener una medida precisa de cuánto debe comer su mascota. Se pueden utilizar frutas y verduras saludables bajas en calorías como premio. Varias opciones incluyen rodajas de manzana, zanahorias, apio y pepino. Evite las uvas, las pasas, la cebolla, el ajo y los aguacates, ya que pueden ser muy tóxicos.
El ejercicio es un componente muy importante para lograr la pérdida de peso. Por lo tanto, agregar más tiempo de juego, caminatas frecuentes y posiblemente incluso una cinta de correr para gatos puede ayudar a lograr los objetivos de pérdida de peso de su mascota. Los pesajes frecuentes también son un componente muy importante para la pérdida de peso para realizar un seguimiento de la progresión del peso de su mascota.
Si sospecha que su mascota tiene sobrepeso, comuníquese con su veterinario para que pueda analizar la mejor opción para su mascota.
De ‘Fat Vincent’ a ‘Skinny Vinny’
En 2016, un perro salchicha obeso de 7 años llamado Vincent fue entregado a un refugio de animales en Houston, Texas, después del fallecimiento de su dueño. Pesaba 38 libras. Gracias a la ayuda de K-9 Angels Rescue, pudo perder más de la mitad de su peso corporal y pasó a llamarse Skinny Vinny. Pesó 17 libras después de un viaje de pérdida de peso de 8 meses.
By Dr. Angélica Calderón
Cat image: Jami430, CC BY-SA 4.0, via Wikimedia Commons
Diabetes in Cats: Prevention and Treatment

Diabetes mellitus is a condition in which the body cannot properly produce or respond to the hormone insulin. Insulin regulates the amount of glucose (sugar) in the bloodstream and delivers glucose to the tissues of the body to use as energy. Diabetes results in elevated levels of glucose in the blood. The most common form of diabetes in cats is type 2 diabetes. In type 2 diabetes, glucose levels are high because cells in the body do not respond appropriately to insulin.
Diabetes is the second most common endocrine disease in cats. (The body’s endocrine system consists of several glands—in the case of diabetes, that gland is the pancreas—that make hormones, which are chemical messengers to control organs throughout the body.)
Cats are typically diagnosed with diabetes between the ages of 10 and 13 years. More cats are acquiring diabetes as the number of overweight or obese cats grows. The average cat that weighs 13 pounds or more has about four times the risk of developing diabetes as a smaller cat. Signs of diabetes can include increased thirst, increased urination, weight loss, and increased appetite.
Diagnosis
When a cat is suspected of having diabetes, a veterinarian will perform blood and urine testing. Diabetes is indicated if blood testing shows an elevated glucose level (hyperglycemia) and urine testing shows evidence of glucose in the urine (glucosuria).
Because stress in cats can lead to both hyperglycemia and glucosuria, another confirmation test called fructosamine is usually done. Fructosamine concentration reflects the average glucose concentration for the past 1 to 2 weeks and is not impacted by stress. If this test comes back as elevated, the diagnosis of diabetes is confirmed.
Treatment
Insulin is the treatment of choice for cats with diabetes. This typically requires twice daily administration. In addition, dietary management can be an important component of managing diabetes in cats. A high-protein/low-carbohydrate diet is recommended. Weight loss is also an important component of diabetic management in overweight cats. Weight loss, if attempted, should ideally be gradual, one-half percent to 1% of total body weight lost per week.

The goals of treatment are to maintain a healthy blood glucose, stop or control unintended weight loss, stop or control increased thirst and urination, and avoid hypoglycemia (low blood glucose).
Unlike dogs, cats can reach diabetic remission; these cats have near-normal blood glucose levels without receiving insulin or other blood-sugar–lowering medication. However, cats in diabetic remission require close monitoring to ensure that they do not relapse. Remission is not achievable in every diabetic cat.
Monitoring
Blood glucose curves are used to monitor response to insulin dosing. If a blood glucose curve is performed at home, pet owners measure the first blood glucose reading before the insulin injection. Then, they test every 2 to 4 hours until the next dose of insulin, depending on the type of insulin used. Performing curves at home eliminates the stress of coming to the clinic, which can affect the accuracy of the testing. Owners may need to perform a blood glucose curve several times to find the right dose for their cat.
One method of measuring glucose is by using a glucose meter calibrated for feline blood, such as a AlphaTRAK3. Another way is by using a continuous glucose monitor, such as a FreeStyle Libre. These monitors can be picked up at a human pharmacy and installed by a veterinarian or veterinary technician. Other important monitoring tests include serial bloodwork and urine testing. Your veterinarian will help determine the frequency at which these tests should be performed.
Monitoring your cat’s level of thirst and urination, weight, and appetite are important throughout treatment. These measures can give clues as to how well the diabetes is being managed. Unfortunately, monitoring response to treatment in diabetic cats can be frequent and expensive.
Complications of Diabetes
One complication of diabetes is diabetic ketoacidosis (DKA). This problem occurs when there is not enough insulin in the body to control the amount of glucose in the blood. DKA happens in uncontrolled diabetics. Without the proper amount of insulin in the body, glucose cannot be used as an energy source. Instead, the body breaks down fat, which produces ketone bodies. With high levels of ketones, the body becomes more acidic, which disrupts fluid and electrolyte balance. Left untreated, the resulting abnormal electrolyte balance may lead to abnormal heart rhythms and muscle function and death. Signs of DKA can include increased thirst or urination, lethargy, weakness, vomiting, increased respiratory rate, decreased appetite, and weight loss.
The other complication is hypoglycemia, or low blood sugar, which may arise when insulin therapy lowers the blood sugar significantly. Signs of hypoglycemia include weakness, lethargy, vomiting, lack of coordination, seizures, and coma. Hypoglycemia can be fatal if left untreated. A diabetic cat that shows any of these signs should be offered its regular food immediately. If the cat does not eat voluntarily, it should be given oral glucose in the form of honey, corn syrup, or dextrose gels and brought to a veterinarian immediately. However, if a cat is seizing or comatose, oral glucose methods should not be attempted.
If you’ve noticed changes to your cat’s eating and drinking habits as well as weight, please have them seen by a veterinarian for additional testing to be done as soon as possible.
By Jeanette Barragan, DVM
¿Qué hacer cuando su gato(a) hace del baño afuera de su caja?

Photo by Luku Muffin on Unsplash
¡Orinar o defecar fuera de la caja de arena puede ser muy frustrante para todos! También puede ser la primera, y a veces la única, señal de que algo anda mal. Se recomienda encarecidamente una visita al veterinario cada vez que haya un comportamiento inusual en nuestras mascotas, particularmente la micción inapropiada. Mientras tanto, considere lo siguiente:
Todos los gatos necesitan satisfacer sus necesidades básicas. Sin embargo, cuando hay varios gatos en el hogar, es particularmente importante asegurarse de que haya muchos recursos en forma de cajas de arena, estaciones de alimentación, espacios verticales, estaciones para dormir, escondites y tazones de agua. El castigo es ineficaz y confuso para los gatos. El entrenamiento basado en recompensas ayuda a mejorar la comunicación al tiempo que proporciona estimulación mental e interacción humana positiva. Los juguetes dispensadores de alimentos y rompecabezas imitan la caza y fomentan la exploración de su ambiente, reduciendo los niveles generales de estrés y satisfaciendo las necesidades básicas.
Los modelos generales que le ayudarán a satisfacer las necesidades básicas de la caja de arena incluyen las siguientes sugerencias:
- Tenga una caja de arena más que gatos para que los gatos más quisquillosos puedan encontrar una caja limpia. ¡La regla es 1 caja de arena por gato más una extra!
- La ubicación importa: los gatos prefieren un área tranquila y aislada, lejos de electrodomésticos ruidosos, hornos, aire acondicionado y áreas de tráfico pesado.
Considere el uso de feromonas como Feliway para reducir el estrés si ha tenido cambios recientes dentro del hogar (nuevo bebé o mascota, mudanza, visitas, etc.) - El tamaño importa: las cajas de arena deben ser al menos 1.5 veces la longitud del cuerpo del gato y aproximadamente 3 veces más anchas que el gato.
¡Considera crear una nueva caja de arena a partir de un contenedor de almacenamiento si no puedes encontrar una lo suficientemente grande! Las cajas de suéteres debajo de la cama son excelentes cajas de arena.(YouTube tiene muchos videos geniales DIY)
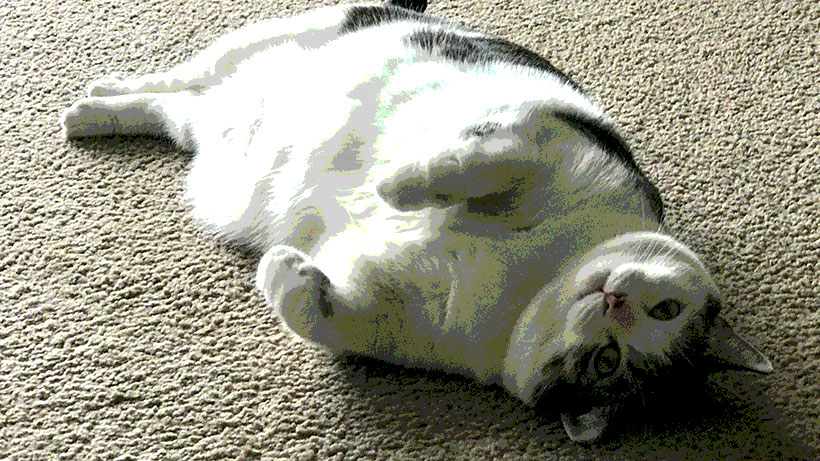
El aumento de peso y la obesidad es un gran problema para nuestros amigos felinos. Además de dificultar encontrar una caja lo suficientemente grande, el exceso de grasa afecta negativamente a la salud y la longevidad de un gato. Tienen un mayor riesgo de cáncer, diabetes y problemas cardíacos. También son propensos a la artritis y a una degeneración más rápida de las articulaciones afectadas: ¡puede doler saltar a la caja o adoptar la postura para ir al baño! - Saca la caja varias veces al día.
- Incluso con arenas aglomeradas, deseche la caja al menos una o dos veces por semana.
- Lave la caja semanalmente, enjuague bien y seque al aire para eliminar cualquier olor del agente de limpieza. El agua caliente y el jabón son los mejores para la limpieza.
- No use arena perfumada, revestimientos o aditivos como bicarbonato de sodio.
- Si al gato le gusta cavar, haz que la arena sea profunda. Si el gato sacude la arena de sus patas, haz que la arena sea poco profunda o cambia a un tipo diferente (aserrín granulado, trigo sarraceno, etc.).
- Lavar, enjuagar y secar cualquier área que el gato haya ensuciado fuera de la caja y luego use un buen removedor de olores. Los mejores ayudan a descomponer enzimáticamente los compuestos de la orina y hacen que algunos odorantes sean demasiado pesados para ser inhalados. NO use lejía ni productos pesados similares.
- De todos modos, siga al gato y vea lo que elige, imite esa elección.
Are You Finding Pee or Poop Outside the Litter Box?
Urinating or defecating outside the litter box can be very frustrating for all! It can also be the very first, and sometimes only, sign that something is wrong. A veterinary visit is highly encouraged any time there is unusual behavior in our pets, particularly inappropriate urination.

In the meantime, consider the following:
All cats need their basic needs met. However, when there are multiple cats in the household, it is particularly important to make sure there are plenty of resources in the form of litter boxes, feeding stations, vertical spaces, sleeping stations, hiding areas, and water bowls. Punishment is ineffective and confusing for cats. Reward-based training helps to improve communication while providing mental stimulation and positive human interaction. Food dispensing and puzzle toys mimic hunting and encourage exploration of their environment, reducing overall stress levels and meeting basic needs.
General guidelines that will help you meet the basic litter box needs include the following suggestions.
- Have one more litter box than you have cats so that fussier cats can find a clean box. The rule is 1 litter box per cat plus an extra!
- Location matters: cats prefer a quiet, secluded area away from loud appliances, furnaces, air conditioning, and heavy traffic areas.
Consider using pheromones like Feliway for stress reduction if you have had recent changes within the household (new baby or pet, moving, visits, etc.) - Size matters: litter boxes should be at least 1.5 times the length of the cat’s body and about 3 times as wide as the cat so the cat can move and turn around.
Consider creating a new litter box out of a storage bin if you cannot find one big enough! Underbed sweater boxes make great litter boxes. (YouTube has many great DIY videos.)
Weight gain and obesity is a huge problem for our feline friends. Apart from making it difficult to find a box that is big enough, excess fat negatively impacts a cat’s health and longevity. Heavy cats are at a higher risk for cancer, diabetes, and heart issues. They are also prone to arthritis and faster degeneration of the affected joints. It may hurt to jump into the box or posture to potty! - Scoop the box multiple times a day.
- Even with clumpable litters, dump the box at least once or twice a week.
- Wash the box weekly, rinse well, and air dry to remove any odor of the cleaning agent. Hot water and soap are best for cleaning.
- Do not use scented litter, liners, or additives like baking soda.
- If the cat likes to dig, make the litter deep. If the cat flicks the litter from his or her feet, make the litter shallow or switch to a different type (pelleted sawdust, buckwheat, etc.).
- Wash, rinse, and dry any area the cat has soiled outside the box and then use a good odor eliminator. The best ones help to enzymatically break down urine compounds and make some odorants too heavy to be sniffed. Do NOT use bleach or similar heavy products.
- Regardless, follow the cat around and see what that cat chooses – mimic that choice.
—Dr. Ana Valbuena
Vaccines in Dogs and Cats / Vacunas en Perros y Gatos

“Prevention is cheaper than treatment.” A quote that I will forever remember from Dr. Vinu, a primary care veterinarian I worked for during my undergraduate studies at the University of Illinois-Chicago.
Vaccines are very critical in cats and dogs, and the vaccine series are started at a very young age. Some vaccines even need to be boosted in order for the pet to reach adequate immunity.
There are many different vaccines in cats and dogs. Some vaccines are core vaccines, meaning that they are recommended in every patient, and some are considered lifestyle vaccines, meaning that it depends on what your pet does.
Is your dog frequently boarded at a boarding facility or often goes to grooming, where they might be surrounded by many other dogs? Does your dog go to forest preserves or on camping trips where they can be exposed to ticks? Is your cat a strictly indoor cat or an indoor/outdoor cat?
All of those are great questions that are usually asked at the beginning of your annual wellness exam. Yes, we may ask many, many questions during your pet’s wellness exam, but we are putting the puzzle pieces together to recommend the best vaccine schedule for your pet.
Rabies Vaccine in Dogs AND Cats
Having your pet vaccinated for rabies is required by law. It is recommended that the canine and feline rabies vaccine be administered at 4 months of age. However, it is sometimes given earlier in a shelter setting. The first rabies vaccine is usually a 1-year vaccine, while the following year your pet can get either the 1-year or 3-year vaccine.
Rabies is transmitted via bite wounds, usually by wildlife like skunks, bats, racoons, and foxes. The virus attaches to local muscle cells, then penetrates local nerves and ascends to the brain.
There is no reliable effective treatment for rabies. Infection usually results in death of the animal. Once clinical signs are present, death can occur within 10 days.
If your pet bites another animal or human and is not up to date on their rabies vaccine, depending on their vaccine history, they might have to be confined and observed at a veterinary facility for 10 days. If the animal shows any symptoms or there is suspicion that the pet might have rabies, their brain tissue must be submitted for sampling. This means that they must be humanely euthanized for tissue submission.
Regulations can vary by state or county, so it is important to keep up with current regulations. Visit rabiesaware.org for more information regarding regulations in your area. Ultimately, prevention consists of vaccination as well as limiting exposure to wildlife. Please visit your local veterinarian if your pet is not up to date on the rabies vaccine.
Vaccines in Dogs: Distemper (DAPP)
The second core vaccine in dogs is the distemper vaccine (DAPP). This vaccine protects against the Distemper Virus, Parvovirus, Adenovirus 1 & 2, and Parainfluenza virus. The DAPP vaccine is started at 8 weeks of age and must be boostered at least 3 times, 3 to 4 weeks apart.
This means that your puppy will get a DAPP vaccine at 8 weeks,12 weeks, and 16 weeks old. After the initial puppy series, the vaccine becomes annual. It is also available in a 3-year version, which can be the year after your puppy’s initial vaccine series.
Parvovirus is a common viruses affecting puppies. Any puppy with clinical signs consisting of vomiting and diarrhea should be tested for parvovirus. A diagnosis can be made from a fecal sample.
Intensive supportive care is needed to treat a dog that has been infected with parvovirus. Supportive care consists of hospitalization, fluid therapy, antibiotics, anti-nausea medication, anti-diarrheal medication, and monitoring blood work changes (particularly your dog’s white blood cells). Be prepared for a 5- to 7-day hospitalization as well as an expensive bill, depending on the severity of your dog’s illness.
Without treatment, this virus can be fatal. Prevention is cheaper than treatment.
Vaccines in Dogs: Leptospirosis
Although the canine Leptospirosis vaccine is not a core vaccine, it is highly recommended in areas that have a high rodent population. It can be given as early as 12 weeks of age and needs to be boostered 3 to 4 weeks after an initial dose is given. After that, it is given annually.
Dogs can become infected with this bacterium via open wounds or mucus membranes coming into contact with infected urine or infected water or soil. This bacterium can survive for weeks to months in the environment, so it is important to have your pet vaccinated if you live in an area that has a high rodent population.
Leptospirosis is zoonotic, which means that humans can get infected as well. An infection can quickly lead to organ damage and can affect the kidneys and liver. Clinical signs can be very nonspecific, and treatment consists of antibiotics and supportive care. In severe cases infection can lead to irreversible organ damage.
Vaccines in Dogs: Bordetella
The canine Bordetella vaccine covers Canine Kennel Cough. It requires no booster and is given annually, although in some cases it is recommended to be given every 6 months. It can be delivered either intranasally or subcutaneously.
Bordetella is essentially an infectious bronchitis and is spread within respiratory secretions from an infected dog. In crowded situations with many animals, for example, at a boarding or grooming facility, dogs can be more predisposed to infection due to close contact as well as poor ventilation.
Clinical signs can range from mild to severe symptoms, such as a hacking cough and pneumonia. Treatment consists of antibiotics and quarantine. Keep in mind that many boarding and grooming facilities require this vaccine.
Vaccines in Dogs: Canine Influenza Virus
The canine influenza virus (CIV) vaccine requires one additional booster given 3 to 4 weeks after the initial dose. After that, it is given annually. It can be started as early as 16 weeks old.
Clinical signs can be very similar to Bordetella and can include cough, sneezing, and nasal discharge. Outbreaks are most commonly associated with kennels where dogs are in close contact. This virus is spread via nasal secretions. It can be hard to distinguish Bordetella from CIV, so treatment consists of controlling secondary signs and treating symptomatically. That means antibiotics and cough suppressants, depending on the severity.
Vaccines in Dogs: Lyme Disease
The canine Lyme vaccine is a lifestyle vaccine for dogs that frequently go to forest preserves or camping. If you live in a highly wooded area, this vaccine is highly recommended due to tick exposure. It can be given any time after 16 weeks of age and requires one additional booster 3 to 4 weeks after the first dose. After that, it is an annual vaccine.
Lyme disease is spread via a bite from infected ticks. Lyme disease can be diagnosed with a SNAP 4DX heartworm test, which entails a blood sample from your dog. Results are obtained in no more than 8 minutes. However, a positive Lyme result does not differentiate exposure to the disease from active infection.
Clinical signs can vary and can be very nonspecific. These can include fever, fatigue, and swollen joints. Treatment consists of antibiotics and managing secondary symptoms. Don’t forget your dog’s monthly flea and tick preventatives, which can greatly reduce the chance of infection with Lyme disease.

Vaccines in Cats: FVRCP
The Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia (FVRCP) vaccine series, also called the cat distemper vaccine, should be started at 6 to 8 weeks of age. This is boostered every 3 to 4 weeks until your kitten is 16 weeks old. This vaccine is also available in a 3-year version that can be given the year after your kitten’s initial vaccine series.
Feline panleukopenia is similar to parvovirus in dogs. It is a very contagious and life-threatening infectious disease that can spread among cat colonies or cats housed with many other cats. An infected cat sheds the virus via secretions, e.g., feces, vomit, urine, saliva, and mucus membranes. Infection occurs when the virus enters through the nose or mouth.
The virus suppresses the immune system and depletes the cat’s white blood cells, leaving the infected individual immunosuppressed and vulnerable to other infectious diseases. Clinical signs can be nonspecific and include fever, vomiting, diarrhea, and lethargy.
Similar to parvovirus in dogs, treatment of a cat infected with panleukopenia consists of hospitalization, aggressive fluids therapy, antinausea and anti diarrheal medications, and supportive care.
Vaccines in Cats: Feline Leukemia Virus
If your cat is an indoor/outdoor cat, the feline leukemia vaccine is highly recommended due to socialization with other cats. This vaccine requires an additional booster 3 to 4 weeks after initial dose.
Feline leukemia virus (FLV) is spread through close social contact with saliva, blood, urine, or feces. There is no effective treatment, so treatment consists of supportive care. Prognosis after infection can be variable.
One Last Reminder
Vaccinating your dogs and cats is very important. If your pet is not up to date on vaccines or their annual wellness exam, please schedule an appointment with their primary care veterinarian to get their vaccines updated.
And remember, prevention is cheaper than treatment.
—Dr. Angelica Calderon

Vacunas en Perros y Gatos
La prevención es más barata que el tratamiento. Una cita que siempre recordaré del Dr. Vinu, una veterinaria con la que trabajé durante mis estudios en la UIC.
Las vacunas son muy críticas en gatos y perros y sus series se inician a una edad muy temprana, incluso algunas vacunas necesitan ser reforzadas para que la mascota alcance la inmunidad adecuada. Hay muchas vacunas diferentes en gatos y perros. Algunas vacunas son vacunas básicas, lo que significa que se recomiendan para todos los pacientes, y otras se consideran vacunas de estilo de vida, lo que significa que depende de lo que haga su mascota. Su perro se aloja con frecuencia en un centro de alojamiento o va frecuentemente a la peluquería, donde puede estar rodeado de muchos otros perros? Su perro va a reservas forestales o a viajes de campamento donde puede estar expuesto a las garrapatas? Su gato es un gato estrictamente de interior o un gato de interior/exterior? Todas esas son excelentes preguntas que generalmente se hacen al comienzo de su examen anual de bienestar. Sí, es posible que le hagamos muchas preguntas durante el examen de bienestar de su mascota, pero estamos reuniendo las piezas del rompecabezas para recomendar el mejor programa de vacunas para su mascota.
Vacuna contra la Rabia en Perros y Gatos
La ley exige que su mascota sea vacunada contra la rabia. Se recomienda que la vacuna contra la rabia canina y felina se administre a los 4 meses de edad, sin embargo, a veces se puede administrar antes en un refugio. La primera vacuna suele ser una vacuna de 1 año, sin embargo, al año siguiente, su mascota puede recibir la vacuna contra la rabia de 1 año o de 3 años.
La rabia se transmite a través de heridas por mordedura, generalmente por la vida silvestre como zorrillos, murciélagos, mapaches y zorros. El virus se adhiere a las células musculares locales y luego penetra en los nervios locales y asciende al cerebro. No existe un tratamiento eficaz y fiable para la rabia y la infección suele provocar la muerte del animal. Una vez que los signos clínicos están presentes, la muerte puede ocurrir dentro de los 10 días. Si su mascota muerde a otro animal o humano y no está al día con la vacuna contra la rabia, dependiendo de su historial de vacunas, es posible que deba ser confinado y observado en un centro veterinario durante 10 días. Si el animal muestra algún síntoma o se sospecha que la mascota pueda tener rabia, se debe enviar su tejido cerebral para la toma de muestras. Esto significa que deben ser sacrificados humanamente para la presentación de tejido. Las regulaciones pueden variar según el estado o el condado, por lo que es importante mantenerse al día con las regulaciones actuales. Puede visitar rabiesaware.org para obtener más información sobre las regulaciones en su área. En última instancia, la prevención consiste en vacunar y limitar la exposición a la vida silvestre. Visite a su veterinario local si su mascota no está al día con la vacuna contra la rabia.
Vacunas en Perros
Distemper (DAPP):
La segunda vacuna básica en perros es la vacuna contra el distemper(DAPP). Esta vacuna protege contra los virus de distemper, el parvovirus, el adenovirus 1 y 2 y el virus de la parainfluenza. La vacuna DAPP se inicia a las 8 semanas de edad y debe reforzarse al menos 3 veces, con 3-4 semanas de diferencia. Esto significa que su cachorro recibirá la vacuna DAPP a las 8, 12 y 16 semanas de edad. Después de la serie inicial de cachorros, se vuelve anual. Esta vacuna también está disponible en un año 3 que se puede administrar el año siguiente después de la serie inicial de vacunas de sus cachorros.
El parvovirus es uno de los virus más comunes que cubre esta vacuna. Cualquier cachorro con signos clínicos que consisten en vómitos y diarrea debe someterse a una prueba de parvovirus y se puede llegar a un diagnóstico con una muestra fecal. Se necesitan cuidados intensivos para tratar a un perro que ha sido infectado con parvovirus y, en última instancia, el tratamiento es de apoyo. La atención de apoyo consiste en hospitalización, terapia de fluidos, antibióticos, medicamentos contra las náuseas, medicamentos contra la diarrea y el control de los cambios en los análisis de sangre (en particular, los glóbulos blancos de su perro). Esté preparado para una hospitalización de 5 a 7 días, así como para una factura costosa, según la gravedad de los síntomas de su perro. Sin tratamiento, este virus puede ser fatal. La prevención es más barata que el tratamiento.
Leptospirosis:
Aunque la vacuna contra la leptospirosis canina no es una vacuna básica, es muy recomendable en áreas que tienen una alta población de roedores. Puede administrarse tan pronto como a las 12 semanas de edad y debe reforzarse 3 o 4 semanas después de administrar la dosis inicial. Después de eso, se da anualmente.
Los perros pueden infectarse con esta bacteria a través de heridas abiertas o membranas mucosas que entran en contacto con orina infectada o agua o tierra infectada. Esta bacteria puede sobrevivir durante semanas o meses en el medio ambiente, por lo que es importante vacunar a su mascota si vive en un área con una gran población de roedores. La leptospirosis es zoonótica, lo que significa que los humanos también pueden infectarse. Esto puede conducir rápidamente a daños en los órganos y puede afectar los riñones y el hígado. Los signos clínicos pueden ser muy inespecíficos y el tratamiento consiste en antibióticos y atención de apoyo; sin embargo, en casos graves, puede provocar daños irreversibles en los órganos.
Bordetella:
La vacuna canina Bordetella cubre la tos canina. No requiere refuerzo y se administra anualmente, sin embargo en algunos casos se recomienda administrar cada 6 meses. Hay dos formas disponibles, por vía intranasal y por vía subcutánea.
Bordetella es esencialmente una bronquitis infecciosa y se transmite dentro de las secreciones respiratorias de un perro infectado. En situaciones de hacinamiento donde hay muchos animales en una instalación, por ejemplo, alojamiento o aseo, los perros pueden estar más predispuestos a la infección debido al contacto cercano y a la mala ventilación. Los signos clínicos pueden variar desde síntomas leves a graves, como tos seca, hasta neumonía. El tratamiento consiste en antibióticos y cuarentena durante el tratamiento. Tenga en cuenta que muchas instalaciones de alojamiento y aseo requiere esta vacuna.
Virus de la influenza canina (CIV):
La vacuna contra el virus de la influenza canina requiere un refuerzo adicional administrado de 3 a 4 semanas después de la primera dosis inicial, luego de lo cual se vuelve anual. Se puede iniciar desde las 16 semanas de edad.
Los signos clínicos pueden ser muy similares a los de Bordetella y pueden incluir tos, estornudos y secreción nasal. Los brotes se asocian más comúnmente con perreras donde los perros están en contacto cercano con otros perros y este virus se transmite a través de las secreciones nasales. Puede ser difícil distinguir Bordetella de CIV, por lo que el tratamiento consiste en controlar los signos secundarios y tratar sintomáticamente. Eso significa antibióticos y supresores de la tos, según la gravedad.
Lyme:
La vacuna canina de Lyme es una vacuna de estilo de vida. Esto significa que si tu perro va con frecuencia a reservas forestales o a acampar, o si vives en una zona muy boscosa, es muy recomendable debido a la exposición a las garrapatas. Se puede administrar en cualquier momento después de las 16 semanas de edad y requiere un refuerzo adicional de 3 a 4 semanas después de la primera dosis inicial. Después de eso, es una vacuna anual.
La enfermedad de Lyme se transmite a través de una picadura de garrapatas infectadas. La enfermedad de Lyme se puede diagnosticar con una prueba de gusano del corazón SNAP 4DX, que implica una muestra de sangre para su perro. Los resultados se obtienen en no más de 7-8 minutos. Sin embargo, incluso si su perro tiene un resultado positivo de Lyme, eso no diferencia la exposición frente a la infección activa. Los signos clínicos pueden variar y pueden ser muy inespecíficos. Estos pueden incluir fiebre, fatiga, articulaciones inflamadas, etc. El tratamiento consiste en antibióticos y el control de los síntomas secundarios. No olvide los preventivos mensuales contra pulgas y garrapatas de sus perros, ya que pueden reducir en gran medida la posibilidad de infección con la enfermedad de Lyme.

Vacunas en Gatos
FVRCP:
La serie de vacunas FVRCP (moquillo felino) debe comenzar a las 6-8 semanas de edad. Esta vacuna requiere refuerzos y se refuerza cada 3-4 semanas hasta que tu gatito tenga 16 semanas. Esta vacuna también está disponible en un año 3 que se puede administrar el año siguiente después de la serie inicial de vacunas de sus gatitos.
FVRCP significa rinotraqueítis viral felina, calicivirus y panleucopenia. La panleucopenia felina es similar al parvovirus en perros. Esta es una enfermedad infecciosa muy contagiosa y potencialmente mortal que puede afectar a las colonias de gatos o a los gatos alojados con muchos otros gatos si una persona está infectada. Un gato infectado elimina el virus a través de secreciones, que incluyen heces, vómito, orina, saliva y membranas mucosas. La infección se produce cuando el virus entra por la nariz o la boca. El virus suprime el sistema inmunológico y agota los glóbulos blancos del gato, dejando al individuo infectado inmunosuprimido y vulnerable a otras enfermedades infecciosas. Los signos clínicos pueden ser inespecíficos e incluyen fiebre, vómitos, diarrea y letargo. Similar al parvovirus en perros, el tratamiento de un gato infectado con panleucopenia consiste en hospitalización, fluidoterapia agresiva, así como antináuseas, antidiarreicas y atención de apoyo.
Virus de la leucemia felina
Si su gato es un gato de interior/exterior, la vacuna contra la leucemia felina es muy recomendable debido a la socialización con otros gatos. Esta vacuna requiere un refuerzo adicional de 3 a 4 semanas después de la dosis inicial.
FeLV (virus de la leucemia felina) se propaga a través del contacto social cercano con saliva, sangre, orina, heces. No existe un tratamiento eficaz, por lo que el tratamiento consiste en cuidados de apoyo. El pronóstico después de la infección puede ser variable.
Es muy importante vacunar a sus perros y gatos. Si su mascota no está al día con las vacunas o su examen anual de bienestar, programe una cita con su veterinario de atención primaria para actualizar sus vacunas.
Y recuerda, la prevención es más barata que el tratamiento.
—Dr. Angelica Calderon
Hyperthyroidism in Cats: Is This Why Your Older Cat Is Skinny?
Hyperthyroidism is the most common endocrine disease in middle-aged and senior cats. It is typically diagnosed when the cat is 12 to 13 years old.
Like the name implies, hyperthyroidism is the increased production and secretion of thyroid hormones from an abnormally functioning and enlarged thyroid gland. Because thyroid hormones affect almost every organ in a cat’s body, having excessive hormones typically causes secondary health issues, such as heart disease and high blood pressure. Hyperthyroidism can also mask kidney disease in cats.
In most cases, this disease is caused by a non-cancerous tumor, called an adenoma, on the thyroid gland. The exact cause of this disease in cats is not currently known.
Clinical Signs and Diagnosis
The most common sign of hyperthyroidism is weight loss in the face of an increased appetite. Over time, a cat with hyperthyroidism will become increasingly skinnier and may also lose muscle mass.
These cats may also experience increased thirst and urination, changes to their hair coat quality (more greasy, matted, or unkempt), vomiting, diarrhea, and increased vocalization.
Diagnosis of hyperthyroidism is through a complete physical examination as well as lab testing (complete blood count, chemistry, urinalysis, and thyroid hormones). If cat has hyperthyroidism, a thyroid hormone called T4 will be elevated on these lab tests.
Treatment
There are currently four methods of treatment for hyperthyroidism; all have the goal of returning thyroid hormone levels to normal. Treatment options include medical therapy with antithyroid drugs; dietary therapy with iodine-restricted diets; surgical removal of the thyroid gland; and radioactive iodine therapy.
Medical Therapy
Methimazole is the most common anti-thyroid medication. It reduces the production and release of thyroid hormone from the thyroid gland. This therapy does not serve as a cure for the disease but allows for control.
Methimazole is relatively inexpensive and is either administered orally or as a transdermal gel that is applied to the ear. Both forms of medication are given twice a day. Some cats experience side effects of this medication within the first few months of starting it. These include vomiting, decreased appetite, lethargy, and skin itchiness that causes the cat to scratch and wound their face.
While on methimazole, repeated blood monitoring must be done to ensure the proper dosage is being used as well as to monitor kidney function and overall health. During the first 2 to 3 months of treatment, lab testing is done every 2 to 3 weeks. After thyroid hormone levels have normalized, monitoring is then done every 3 to 6 months.
Dietary Therapy
Feeding an iodine-restricted diet is another therapeutic option. This approach works because iodine is needed for the body to produce thyroid hormones. For the best results, this diet must be fed exclusively and consistently. These diets have been shown to reduce the levels of thyroid hormones in 3 to 4 weeks. If normal thyroid hormone levels are not achieved within 12 weeks, a different form of treatment is usually selected. Dietary therapy is not effective if the cat does not like to eat the food or regularly has access to other forms of food.
Surgery
Removal of the thyroid glands is another form of treatment. It is a straightforward procedure for a skilled surgeon and has a good success rate. Surgery has the advantage of being curative and eliminating the need for long-term medication administration. A risk of surgery is accidental damage to the parathyroid glands, which are located close to the thyroid glands. If the parathyroid glands are damaged, the cat’s body will have difficulty producing calcium. Because less invasive treatment options are available, surgery is rarely selected for treatment.
Radioactive Iodine Therapy
Radioactive iodine therapy is currently considered the treatment of choice for cats with hyperthyroidism. Radioactive iodine is given as an injection, which then travels through the bloodstream to the thyroid gland. The radiation from the radioactive iodine then destroys the abnormal thyroid tissue without damaging the surrounding healthy tissue.
The radioactivity does not harm the cat but does pose a risk for humans. Due to this, cats undergoing this treatment are hospitalized for 3 to 5 days after treatment until the radiation levels are low. Cats are not allowed visitors during this time. In 95% of cases, this treatment is curative within 3 months. If not successful, the treatment can be repeated. In rare cases, a cat can become hypothyroid (producing too low levels of thyroid hormone), which then must be treated with thyroid hormone supplement.
Prognosis
Once hyperthyroidism is diagnosed and a form of treatment is selected, most cats do well. As medical therapy and dietary therapy are not curative, treatment is lifelong in these cases. Surgery and radioactive iodine therapy are considered curative, so lifelong treatment is not needed.
If your cat is experiencing any of the clinical signs mentioned, please reach out to your veterinarian to have your cat tested. If your cat is diagnosed with hyperthyroidism, you and your veterinarian can determine the best treatment option for your cat.
—Jeanette Barragan, DVM
Featured photo by Ekaterina Zagorska on Unsplash
Why Bringing Your Cat to the Vet Is Like an Alien Abduction…

…And What You Can Do to Help
After a decade in practice, I’m thankful I’ve only had to go the hospital for a cat bite once. Since then, I’ve gained a lot of experience and understanding of the feline psyche, and my best summation of how cats perceive going to the vet is this: It’s an alien abduction.
Think about it. For the most part, cats live their whole lives in a relatively small area, and an overwhelming majority of them love it that way.
The most important aspect of a cat’s life is their territory (which includes you). Their territory is their world, their home planet.
Most cats rarely travel in cars and only ever see a travel carrier when they are headed to the vet. Imagine, you’re living your life on your home planet, then you are forced into a pod, and thrust into a metal vessel, and taken to a faraway place that smells aseptic and strange. While there, a weird, hairless ape pokes and prods you. Then, you are thrust back into the pod, whisked home, and your owner acts like nothing happened.
I’m honestly surprised more cats haven’t attacked me. I’d like to think I’d put up a fight too, if I was abducted by aliens. However, maybe if they had a nice spread out and some calming aromatherapy, I’d be amenable to some polite questioning.
Making the Vet Visit as Low Stress as Possible
So that’s what we try to do for your feline family members. Here at Medical District Veterinary Clinic, we are Fear Free Certified. This means all the staff members here have taken training in how to make the veterinary experience as low stress as possible.
We have cat treats at the ready, Feliway spray aplenty, and a separate cat area. We also have gone to great lengths to learn how cats think and how to read their body language. We understand what’s important to them.
Cats often get a bad rap. People think that cats are aloof and don’t care about anything, but cats care about everything! Please know that we are doing our best to be peaceful and compassionate alien overlords.
Try This at Home
There are a few things you can do as well to make the trip to the vet a little less stressful. The first is getting your furry felines accustomed to the carriers you use to take them places.
Just bringing the carrier out before a vet visit can be a trigger. If you’re able to leave the carriers out, put your cat’s favorite treats or toys in there. This small step can help greatly to reduce your cat’s aversion to the carrier.
You can also try using products like Feliway spray, Composure treats for cats, or Rescue Remedy. If you think your kitty needs something stronger, talk to us and we may prescribe medications to help make the visit less stressful. For more information about eliminating the stress in your cat’s life, The Ohio State University Veterinary College has a wonderful site call the Indoor Pet Initiative with information about dogs and cats.
So remember, next time Fluffy’s wellness exam comes around, you may be envisioning All Creatures Great and Small, but they may be thinking more Schwarzenegger in Predator.
—Alyssa Kritzman, DVM
What Food Is Best for Your Dog or Cat?

This is a question and a discussion that I have with clients daily. And to be honest, it’s a very difficult question to answer. I am going to give you a few tips on how to pick out a food that is best suited for your dog or cat.

Life Stages
I recommend feeding a food based on the life stage of your pet. The four life stages include growth, young adult, mature adult and senior. The below picture helps illustrate the life stages of cats. Canine life stages are pretty similar, but with more variation due to the vast size difference we see in the canine species. The growth life stage is typically done by 6-12 months of age. For cats the growth phase is typically finished by 6-10 months of age and I recommend transitioning to adult food around that time. If you have a puppy or kitten it is very important for proper growth and development to feed a puppy or kitten food. In the same manner as your pet is aging feeding a senior diet is important as they have different nutrient profiles.
You may ask what about an “All Life Stages” dog or cat food. For a company to market their food as “All Life Stages” the food must meet the nutritional requirements for all life stages. Therefore, most of these foods are formulated as a puppy/kitten food because puppies and kittens have the highest nutritional requirements of the four life stages. These foods can be good foods and well balanced, but they typically have a high caloric density. Therefore, in my experience, dogs are more likely to become overweight than if they were fed some other diets.
Medical Conditions
Does your pet have any health conditions that require a special diet? Prescription diets can play a vital role in management of many health conditions, including kidney disease, diabetes, obesity, allergies, and feline lower urinary tract disease.
If your pet suffers from a medical condition, diet can manage and help many conditions, so I always recommend considering a prescription diet if you pet has one of the above conditions.
More Expensive Does Not Mean Better
Many pet food companies are great at marketing but might not be as good at formulating diets. You can always look for the Nutritional Advocacy AFFCO (Association of American Feed Control Officials) Statement on each bag or can of food. These statements will tell you if the food has been through a food trial or formulated to meet particular feeding guidelines. The ingredient list should also list all ingredients in decreasing amounts by weight.
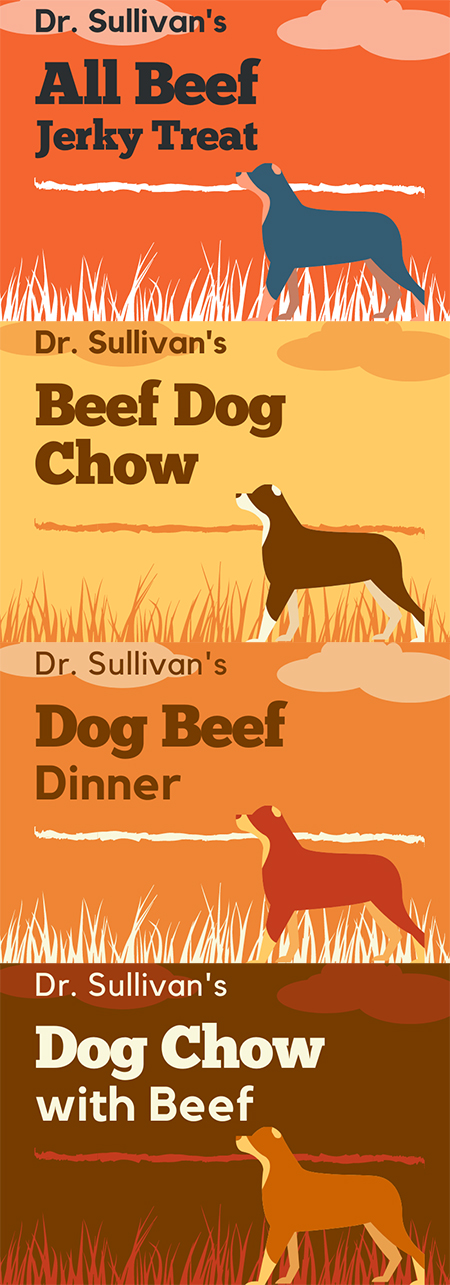
Labels are very confusing and often misleading to consumers. For example, if I made up a food with the following labels, the variation in ingredients can be drastic.
- If the term “All” is used, then the ingredient must make up 100% of product minus preservatives and water. So, this treat would be 100% beef
- If the listed ingredient is used, then the ingredient must make up 95% of product minus water. So, this Beef Dog Chow would be 95% beef on a dry matter basis.
- If the term “dinner,” “platter,” or “recipe” is used, then the ingredient must make up only 25% of product. So, this Beef Dinner is likely only 25% beef.
- If the term “with” is used, then the ingredient must make up only 5% of product. So, this Dog Chow with Beef is likely only 5% beef.
I hope this illustration helps demonstrate how confusing pet food labels can be to both consumers and veterinarians. I recommend visiting the AAFCO website if you want to be better educated about what’s in your pet’s food.
Say No to ‘Grain Free’
Does my pet need grain-free food? The answer is NO. There little to no research showing the true benefit of grain-free food. In fact, grain-free food has been shown to cause heart disease in some dogs. The exact cause is still being researched. Visit this site for more information. https://www.fda.gov/animal-veterinary/animal-health-literacy/questions-answers-fdas-work-potential-causes-non-hereditary-dcm-dogs
What About Raw Food?
Some dogs do really well on raw food, but I do not recommend it. That’s because I see too many owners who try to feed raw but who are not feeding a balanced diet because they are solely feeding raw meat and limited other nutrients.
In the wild canines and felines will consume entire animals. Eating meat, skin, ingesta, organs, and bone makes up a balanced diet.
Raw can be balanced and can be a good diet for some animals, but there is also a public health risk with feeding these diets. This is a statement from the CDC:
“Germs like Salmonella and Listeria bacteria have been found in raw pet food, even packaged ones in stores. These germs can make your pet sick. Your family can also get sick by handling the food or by taking care of your pet.”
Centers for Disease Control and Prevention
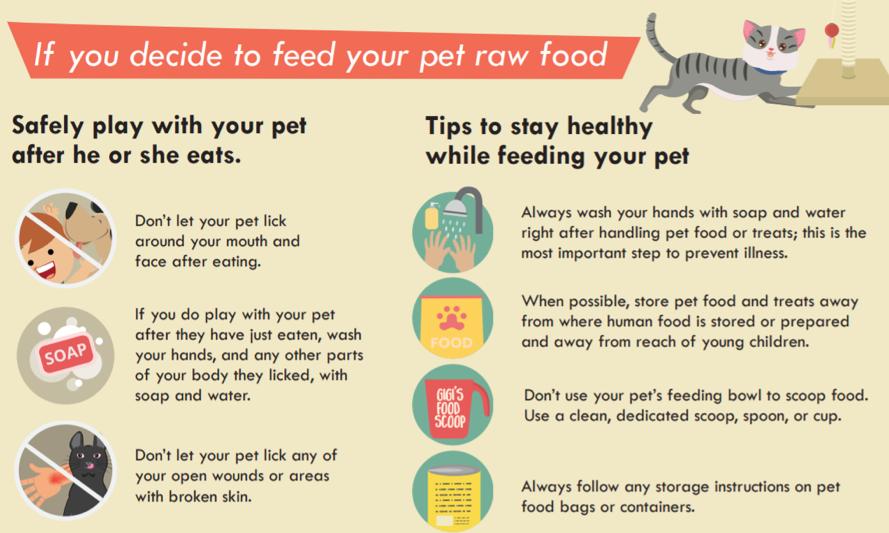
Therefore, if there are young children or anyone who is immune-compromised in your house, I highly advise against feed raw pet foods.
Each Pet Is Different
I hope this information has been helpful and informative. I recommend discussing your pet’s daily calorie needs with your veterinarian as each pet is different, just like people. Two people that have ideal weights of 180 pounds may be able to eat very different diets to maintain their weight, and the same goes for cats and dogs. All 10-pound cats do not need the same daily calories.
The recommendations on the bag or can of food should only be a guide. Some animals may need more calories, but most will need less than the recommended amount to maintain an ideal weight. And always remember to factor in all treats and table scraps into their daily calories. Most pets are overweight these days.
—Dr. Drew Sullivan
Fear Free Practices for Furry Friends

For many people, the doctor’s office can be a scary place. So it is no surprise that many pets view going to the vet with a similar fear.
Our clinic truly believes in Fear Free practices. Our goal is to limit your pet’s stress and fear and make visits with us as pleasant as possible. There are various ways that we do this, which I would like to share with you.
Treats, Teats, and More Treats!
During your pet’s visit you will notice that we like to offer treats. We have biscuits, cheese, peanut butter – like a candy store for dogs and cats! This is not only because we think your pet is adorable and we want to spoil them, but this is also a main way we like to bond with them.
Imagine if you are at the doctor and you are anxiously waiting, and then the doctor walks in and immediately offers you your favorite treat (for me, that would be some delicious baked goods) and socializes with you. You would likely feel much calmer and connected to them. This is the equivalent of what we do with your pets.
Although we have lots of treats, if you have a dog or cat that is pickier with food, please feel free to bring whatever your pet likes best. This is not uncommon, as I have seen many patients that would eat only one food.
We encourage owners to offer treats as well during visits to help make the entire experience as positive as possible. We joke that visits go best when our patients come hungry, so you may want to consider bringing your pet to see us with an empty stomach so there is plenty of space for treats!
Getting on Their Level
We want our patients to feel comfortable, so we often will sit on the ground with them. We hope that by sitting on their level they feel less intimidated and fearful, and that they see us as their “friend.” I have noticed that when I sit on the ground and spend time in the room before even beginning my exam, my patients generally seem more at ease.
Please do not feel obligated to sit with us, but if you would like to you are totally welcome!
Limit Stress from Other Pets
Many cats never leave the home except to go to the vet. They may be stressed by traveling before they even arrive.
The smells and sounds of dogs can be very scary for them, too, which is why we recently created a separate feline waiting room and exam rooms. We use all separate supplies, have tasty treats and fun toys, and have nice feline-friendly smells. In the months since we have started using this new space, I have noticed that cats overall seem much calmer and happier.
Dogs can be become upset from other pets as well. Some of the sweetest and most affectionate dogs that I have met do not get along well with other dogs. Being around other dogs is stressful for them. I personally have a dog-reactive dog, and while she loves people, other dogs make her highly anxious.
To reduce this anxiety, we have multiple tactics, such as choosing specific exam rooms and trying to limit time in the clinic and exam room, when other pets are a trigger for the patient. We also perform exams outside in an isolated area if needed.
Fear Free for Your Pet
Please let us know if your pet is reactive with other pets, or there are any other behavioral concerns, and we will work with you to formulate a plan for their visits.
I hope you can see how much we at Medical District Veterinary Clinic truly care about our amazing patients! We look forward to continuing to make their time with us as fun and enjoyable and fear free as possible!
Amber Slaughter, DVM
The Weather Outside Is Fightful

Oh, what a typical December in a year of continual peace and normalcy.
What’s your favorite holiday memory regarding socially distanced Zoom calls with family members you haven’t seen in person for years due to splintered political realities followed by a deadly pandemic all the while keeping your 6-year-old son inside and away from his friends for 9 months and simultaneously being forced to keep an external facade of sanity and light fun in your two-holiday household while your profession, which is universally adored and undervalued at the same time, is more in demand of your time than at any other period in history?
I have so many.
So we know what usually happens here on the holiday. There is a cute blog post about keeping your dogs and cats safe, titled something like “’Tis the Wheezin’: Asthma During the Holidays.” I have written some in the past (HERE), and feel free to read. It generally can be summed up by this wise adage: “Don’t let your dog and cat eat things or get burned and remember that New Year’s Eve in Chicago generally involves people who do not have children and animals lighting off fireworks late at night to make those of us who do angry.” And don’t buy puppies, kittens, or bunnies as gifts. Instead, buy books like this inspirational tale for the animal lover in your life.
But I’m going to write about an unrelated topic: domesticated cats and the outdoors. I can imagine, even before writing this, that many people have strong feelings about this topic. My intention is not to pass judgment on anyone. I want to just give you the veterinarian perspective, and possibly give you an excuse to see photos of my fat indoor cats sitting next to holiday decorations, because that is how we indoor-cat people are generally seen and heard.

Some cats go outside. Cats go outside because some people feel that they have no choice but to let the cat out. Some people feel that it is philosophically cruel to not let the cat out, and some cats get outside by accident. All are acceptable.
I will be upfront and tell you that my two cats, Crocodile the Russian Blue mutt and Penelope the one-eyed tuxedo, do not go outside. They both try at times and have both gotten out before, but they stay inside and tolerate the complete subservience of all surrounding them.
Some of the dangers facing an outdoor cat are pretty obvious, but let’s go through them (you and I, together, like old friends who aren’t being watched):
1. Fighting with Other Cats
Cat bites and scratches are bad, cause severe infections, and can be fatal. All veterinarians have seen cats brought in with bite wounds that have become severely infected and, at worst, can puncture the abdomen, chest, eyeball, or throat and need surgical fix, hospital stays, and even euthanasia. We clean it up and give antibiotics, but it’s always concerning. This also can lead to:
2. Spread of Infectious Disease
Feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV) are spread through the exchange of bodily fluids (blood, saliva, etc.). Let’s just assume that the cats outside getting into fights are mostly ones that are homeless, and that homeless cats comprise the largest population of cats carrying these viral diseases. Well, the logic chain/train follows, and you see the danger. We can vaccinate for FeLV, so if your cat does go outside, you can get this done. There is no vaccine for FIV. And no treatment for either disease.
3. Other Infectious Disease

Rabies is a classic viral hit and can be spread through other cats or wild animals (bats, skunks, foxes). Make sure your outside cat is vaccinated for rabies, not only because it is the law but also because, even though it is rare, your sweet rabid cat can kill you and your family. (Still waiting for the Hallmark Channel’s Very Special Rabies Christmas.)
Just for fun let’s add endless respiratory infections (that can pass on to the other cats in your house), feline distemper (get your cat vaccinated for that, too), and parasitic diseases such as fleas (get monthly flea protection), ticks (get monthly tick protection), ear mites, intestinal worms (have monthly dewormers given), and ringworm.
All but one of these diseases can be passed on to you, your children, your grandparents, their friends, their friends’ neighbor, your friends’ neighbors’ son’s cat, etc. You see how this works. If you have an outdoor cat, and you’re afraid to tell your veterinarian (which you shouldn’t be), you can still take all the precautions: vaccines, preventatives, etc.
4. And Even More Infectious Disease
For the lucky, cats bring home presents, such as mice, birds, rats, etc. The rodents bring diseases and other rodents. It’s endless.
5. Cats Get Hit by Cars…
… get hit by bikers, get stuck in garages, get hurt by bad people, get snagged on fences, freeze to death, etc. [Cut to unwatchable montage of more horrible things.] It happens.
My previous cat got stuck in someone’s garage. I could not find her and searched for hours around the neighborhood. I eventually heard a cat crying in a garage and called the police who, hours later, located the owner who wasn’t on premise, to open the door. That could have easily gone another way, and I will write that fan fiction novel later.
“Lost cat” signs litter my current neighborhood, and you know they aren’t lost with a hobo bag on a train. They are all either dead, or (at best) living their lives with someone else. Also please have your outdoor cats microchipped. It’s not painful and may save your cats’ lives. You can also buy GPS trackers for their collars. I am not promoting a specific brand, but they are available anywhere.
6. Overpopulation
Cats are really good at making babies, causing the population of stray cats in the city to blow up. These cats either end up being helped by people/shelters that can barely deal with the cats they have or they are left to fend for themselves on the streets to die, starve, or spread more disease.
So first, get your outdoor cat spayed or neutered. It is absolutely the best thing for them, for their health, and to keep down the population of wild cats in need. I also do not need to explain to you how a wild tom cat will treat a sweet young lady cat taking a stroll down the promenade with her uterus and ovaries. If you want to reduce the chances that your boy cat doesn’t get into a fight, well, then neuter. There are conflicting statistics, but most sources suggest that one female cat and her mate and all the subsequent offspring amounts to 11 million cats in nine years.
7. Anti-Nature

Lastly, I fear that some of you feel like the most natural thing for the world is to let your cats outside and let them live the full entirety of their existence. I get this, I really do, but also understand how much destruction to the natural environment cats do. They destroy natural foliage and other wildlife despite their good intentions. There is some very good evidence that the best thing for “nature” is to keep your cats inside, and you can find many other resources on this topic.
There are cats that do better when they go outside. I’ve had clients keep their cats inside and later see them become anxious, yowl, not eat, urinate all over the house, etc. I don’t want your cats to suffer, but if you want to make that transition, there are things we can do. It may not be the case that your cat is anxious because it can’t go outside. In fact, it may be that it has always been anxious, but you never noticed until you kept it inside. Always have us examine your cat before making any judgments. Maybe your formerly outdoor cat is suffering from something else (UTI, pain, etc.).
As always, feel free to discuss with us at any time. This wasn’t meant to be a philosophical treatise on domesticated animals’ rights, though that is generally how I fantasize spending a great deal of my off time.
Try to relax during these times and make sure you don’t feed your dogs chocolate-covered antifreeze-infused garlic balls for the holidays, or give your cats kerosene holiday lamps for Hanukkah.
I will continue to lord over Secret Santas everywhere while I fulfill my long-standing December tradition of making holiday cookies I can’t eat in a house I don’t own.
Be safe, don’t travel, wear masks, and shop locally on-line. And Black Panther is a holiday movie.
— Brett Grossman, DVM
