Our Blog
Prevention Takes the Bite Out of Heartworm Disease

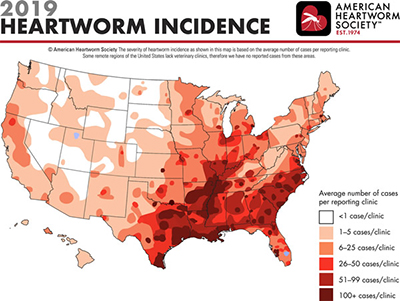
Throughout this time of quarantine, I have been spending more time outside, as I am sure many of you have, too. Besides the overabundance of cicadas in my neighborhood, currently there seems to be a plethora of mosquitoes looking for a blood meal. Just as we love summer in Chicago, so do mosquitoes. Summer is the time for peak transmission of heartworm disease across the U.S. Heartworm disease is considered endemic in Illinois, and according to the American Heartworm Association, clinics in the Chicago area see an average of 25+ cases per year.
As I sit outside, I think how lucky I am because mosquitoes don’t seem to like me; my wife is not so lucky. Then I wonder if my dog, Oskee, is getting bit as much as we are? And is he getting infected with heartworms?
The importance of prevention makes so much sense once you have a little knowledge about the disease process and how monthly preventive medication works. As described in this short video, the monthly preventive does NOT prevent exposure, but kills off any immature baby heartworms already present in your dog. If the preventives are not given every 30 days, the immature heartworms can mature to juvenile worms before the next dose, thus resulting in heartworm disease.
If you miss a dose or are late giving a dose, give the dose as soon as you remember. While uncommon, an infection may develop within your dog from a single missed dose. Multiple missed doses, especially during peak transmission months, puts your dog at high risk of infection.
The heartworm test performed at annual wellness visits screens for adult heartworms. It takes 6 to 7 months after infection for the heartworms to mature into the life stage detected by the heartworm test. Therefore, if you miss a dose, start up prevention as soon as possible. Then have your dog tested within the next year to be sure that infection did not occur during the unprotected period.
For less than $10/month your pet can be protected. While there is a treatment for heartworm disease, it is more expensive and more painful than monthly prevention. The average cost of treatment for a medium-sized dog is $1,500 vs. $10/month for prevention.
If your dog is not currently on prevention or you need a refill, give us a call today. If you have questions about the different preventive medications on the market, please reach out as we would be happy to discuss your questions and concerns.
—Dr. Drew Sullivan
Could COVID Worries Be Bothering Your Pet?

Care for Yourself So You Can Care for Your Pet
Like many of you, I never expected to experience the pandemic we are currently facing. Social distancing, quarantine, virtual gatherings, and isolation have become part of our daily lives due to COVID-19.
Adjusting to this new normal has been challenging for many people. Pets can often sense an owner’s stress and anxiety, which in turn the pets can absorb. Signs of stress in pets can be very subtle, and these behaviors can mimic pets’ normal behavior, so identifying stress can be difficult for owners.
Indicators of stress in dogs include pacing and shaking, whining and barking, trembling, changes in eyes and ears, shedding, panting, changes in bodily functions, hiding, and acting more withdrawn. While cats can exhibit the signs above, they also commonly overgroom (which can lead to sores on the skin) and fail to use the litter box. Cats in particular, are prone to developing urinary symptoms when they are stressed, so it is important that owners keep a close eye on their cat’s litter box habits. It is clear that our mental health impacts our pets, which is one more reason to be mindful of self-care.
Self-care Strategies
In honor of Mental Health Month, here are some strategies to help deal with COVID-related stress:
- Separate what is in your control from what is not. Focus on the things you can do, such as washing your hands, drinking water, and limiting your news consumption (including social media).
- Get outside in nature; fresh air and exercise is beneficial for not only mental health but physical health.
- Challenge yourself to stay in the present. When you find yourself worrying about something that hasn’t happened, gently bring yourself back to the present moment. Try to focus on the positive things happening in your life.
- Stay connected to the people in your life. Reach out to trusted friends and family members when you need support.
- Use meditation and relaxation exercises to promote a sense of calm.
- Eat healthy, well-balanced meals, exercise regularly, and get plenty of sleep.
Enjoy Time with Pets
While many people have transitioned to working from home, pets are enjoying the extra time they get to spend with their owners. You can still enjoy the outdoors with your pets in a safe way by finding quieter and less populated areas. The time outdoors and exercise helps reduce stress and anxiety and is also an opportunity for your dog to have fun and burn off some of their energy.
For your cats, you can find new ways to play with them at home. There are many different types of cat toys available (online shopping is a great way to find some exciting new toys), or you can find some items around the house for the cat to play with. It’s incredible how something as simple as a cotton ball or piece of paper can keep them entertained for hours. This is also a good way to bond with your cat, which is beneficial for mental health.
By taking care of yourself, you will be better able to care for others, including your pets. Although these are uncertain times, we’re in this together!
—Amber Slaughter, DVM
Introducing Telemedicine for Patients

Due to the extended stay-at-home order, starting Monday, April 13, Medical District Veterinary Clinic will offer telemedicine appointments to continue to support our clients.
Please review the following information before you schedule an appointment:
- All telemedicine appointments are for established patients who have been seen within the past 12 months. These patients have a current Veterinary-Client-Patient Relationship (VCPR), making telemedicine a legally acceptable form of care
- Telemedicine appointments can be scheduled for non-emergency sick patients. For example: skin issues, ear infections, lameness, management of chronic conditions, diarrhea, and behavior issues. These appointments will be a convenience for clients, will allow doctors to service more of our clients, and will decrease person-to-person contact.
- Telemedicine appointments can be scheduled:
- If the patient is sick and the client is also sick/quarantined/has been exposed to illness
- If the pet is ill and the client cannot come into the clinic for other reasons
- If the pet’s illness is not emergent but should be discussed with a doctor
- Telemedicine appointments will be available Mondays, Wednesdays, and Fridays, between 8 am and 12 pm. (This may change based on demand.)
- The cost of telemedicine appointments is $30.
- If during the telemedicine appointment, the doctor deems that the pet should be physically seen, the $30 telemedicine fee will still apply. The exam fee for the in-clinic appointment will be discounted to $40 (from $62) if the in-clinic appointment is scheduled and seen within 72 hours of the telemedicine appointment.
Photo by Andrea Piacquadio from Pexels
Curing Your Pet’s COVID-19-Quarantine-Induced Cabin Fever

Because I am a human being living in the third-largest city in the United States, the coronavirus is on my mind. It’s scary, and we all are dealing with our newly realized pandemic anxiety in different ways. Turning to our pets for comfort is natural and nice, but with that also comes a possible increased focus on their every move and well-being.
Some of you have the luxury of being able to self-quarantine with your loved ones, and we all thank you. Some of us still need to be out in the real world saving people, and we all thank you too. This blog post, however, isn’t to inform you about anything related to COVID-19 and human health. For that you can look here. This blog is meant to address your animals’ health during this time.
I know that some of you are worried about your animals getting infected. Though we don’t know everything about this virus, veterinary experts say it is highly unlikely to infect or sicken pets.
What I want to discuss is the quality-of-life needs for your pets, particularly dogs, which depend on social interactions with other dogs and people to relieve boredom and anxiety. All the basic points are applicable to cats too, though the cats that go outside and meet people and other cats are rare.
We are all home (hopefully) now. As much as social interactions need to be at a minimum to help flatten the infectious curve, being outside is not unsafe. Walking your dog is not something you should avoid. In fact, strolling through the streets offers a great opportunity for quiet and reflection. What you need to be careful about, though, is stopping to talk to others and going to dog parks or places where humans congregate. Which in turn means that your dog’s social needs may go unmet.
So how can your dog’s and cat’s cabin fever be remedied?
- Attention. Because you are managing your two children who are home from CPS, trying to keep up on how many celebrities are positive, and Google-deep-diving whether coronavirus can be transmitted through ESP, you may not think that spending 10 minutes here and there playing tug-o-war with your dog is a priority. But don’t underestimate the stress dogs can pick up on. Even a small amount of attention can help them through this.
- Respect boundaries. Though most of your cats and dogs love having you around, it also the case that the sudden increase of bodies home at all times can be a stressor for your 18-year-old cat that is used to the quiet and freedom to sit on the couch alone during your work day and actually enjoy some alone time. I’ve heard from numerous people over recent weeks that they think that their dog and cat may not actually miss them as much as they assumed when they were at work every day. If your animals separate from your space to be alone, it may not mean something is wrong; you just may be annoying. Let them be and make sure there are places for them to retreat to without the clatter of your new bread-making hobby and experimentation with rave-reggae dominating your shared environment.
- Toys. Please don’t run to the store and get a bunch of toys right now, but make the existing toys in your house nice and clean and available. Make toys out of your old clothes or use a discarded water bottle, toilet paper rolls (especially you hoarders), etc. If you Google DIY dog toys, you’ll see a lot of ideas. But be careful you don’t use anything toxic or things that your dogs can swallow. I like this page: https://www.wisebread.com/10-diy-dog-toys-you-can-make-for-pennies
- Train/Teach your dog new tricks. Don’t give up on your sometimes jerk of a dog who stubbornly will not generally or ever listen to you. Don’t as it’s literally and figuratively never too late to try to teach your old dog new tricks. Maybe this is the time you spend teaching her to sit, shake, solve geometry puzzles, speak Turkish, etc. There are tons of trainers who are helping to do things remotely. I plan to have my dog braiding my hair by the summer.
- Go outside. Go outside. Go outside. It may seem contrary to our brains’ frenetic power to actually go in our yard (if you have one) and sit down, but leave your house, walk outside, even though you may need to cross the street to avoid people. You can check Twitter on your front steps with your dog as well as in your living room.
- Divide and comfort. Not all households with multiple animals live in harmony. We have an upstairs cat and downstairs cat. Both are annoyed at the upstairs and downstairs dog. Maybe your herd is split up in different ways. Just like playing tug-o-war with your dogs for 10 minutes could go a long way in fulfilling her needs, try to spend some alone time with each of your animals for a bit. Go upstairs and have a 10-minute pet-fest with your shy cat that hates your power hungry younger cat that generally hogs all the attention.
We all hope this passes soon, though that seems doubtful right now. Read books, play farm hustle, calm yourself, distance. Goodbye.
—Brett Grossman, DVM
We’re Here to Support You
Dear Clients and Patients:
I’m writing to let you know that we are here to help you through this tough time.
While this COVID-19 pandemic disrupts our normal lives, we want to provide you with reassurance that Medical District Veterinary Clinic is available to help when your pet has needs. At the same time, as members of the medical community, we have an obligation to help protect the health and safety of our community.
We as veterinarians have taken an oath not only to protect the health and welfare of animals, but also to promote public health. Currently, we are in a public health crisis, and we want to encourage all our clients to do their part and stay home whenever possible.
Due to this crisis, we are working with limited staff and practicing social distancing wherever possible. We have made the following changes to our procedures so that we can meet our clients’ needs while adhering to guidelines for limiting the spread of COVID-19.
- We are seeing urgent appointments only.
- All owners will be asked to wait in their car during appointments. Doctors will communicate exam findings over the phone and discuss diagnostics.
- Payment will be collected over the phone, and the pet will be returned to the car after procedures are completed.
- Vaccinations:
- Puppy and kitten vaccines: We feel these vaccines are very important to the health and safety of these patients and should be continued on recommended normal schedule.
- Adult pet vaccines: Although vaccines are very important, some vaccinations could be postponed 1 to 2 months, especially for dogs with limited social interaction. If your pet is due for vaccinations, please call us to discuss scheduling options.
- Medication pick-up: Curbside service is now available. The owner will be asked to pay over the phone, and medications will be brought to the car.
Thank you for your understanding as we navigate this difficult time. We hope to resume normal operation in early May and will keep you updated as the situation evolves.
If you need additional resources please refer to our Pet FAQ’s.
Drew Sullivan, DVM
Medical Director
Reduced Service: Seeing Sick Patients Only

The situation is very fluid. Please check this post or our Facebook page for updates.
Last updated March 17.
With recent developments in COVID-19, Medical District Veterinary Clinic is implementing reduced service in order to keep our staff, clients, and community safe. (Remember, your pets are not at risk from COVID-19, but having people bringing their pets to a public place increases the risks for people.)
We will continue to see SICK patients only; wellness and routine procedures will be postponed.
If your pet is due for a crucial vaccine, such as rabies, and your pet goes to daycare or boarding, please contact us to find out if an exception can be made.
If you have a fever, cough, sore throat, or possible exposure to COVID-19, please do not come to the clinic. Arrange for someone else to bring your sick pet to see us.
Stay safe! We all need to work together—but at least 6 feet apart—to implement these public health measures.
Thank you for your understanding and cooperation! We have the best clients in Chicago! ♥
Preparing Your 4-Legged Baby to Meet Your 2-Legged Baby
![[Emmie watches her mom write this blog]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2020/02/Ellie-full.jpg)
There will always be room in Dr. Kritzman’s heart for Emmie, but the space between the baby and the keyboard was getting pretty tight as she wrote this blog.
We all wish—and often expect—that our pets will take to new members of the family easily. We love them, we love our kids, so they should love each other! But adding a new family member that doesn’t do much besides cry (initially) and take away precious belly-rub time can be a huge stressor for our pets.
If you’re like me, you’ve imagined that your pup will be like Nana from Peter Pan. I’ve even had to stop myself from buying that cute hat on Amazon multiple times, because it’s not fair to expect every pet to not only love but like a new baby or child in the family.
It’s a big change. So as I’m counting down the days until our little lady arrives, I thought I’d share just a few tidbits about how to prepare our pets medically and behaviorally for a new arrival.
The Medical
There aren’t many diseases to worry about transmitting from dog or cat to baby, but there are a few you should know about. They are all easily minimized, if not eliminated, with the appropriate care and prevention.
The first are intestinal parasites. Hookworms and roundworms that dogs carry can potentially carry can be spread when exposed skin comes into contact with the larva of these worms or the larva is ingested. The worms grow and can live in the skin or sometimes eye. So it’s important to keep your dogs on a heartworm preventive medication that also covers intestinal parasites. These are monthly preventatives for your dog such as Heartgard Plus or Sentinel Spectrum.
Toxoplasmosis also gets a lot of attention when expectant mothers live with feline family members. Toxoplasmosis is actually pretty difficult to get from cats. You’re more likely to get toxoplasmosis from undercooked pork or contaminated water than from your cat. Cats get toxoplasmosis from eating infected wildlife, so for most indoor-only domestic felines, the likelihood is very low. To play it safe, follow a few simple rules:
- Clean the litter box once a day: it takes longer than 24 hours sitting in stool for toxoplasmosis to become infectious, so if you scoop once a day or more, it shouldn’t be a problem.
- Keep your cat indoor only: if they can’t eat infected wildlife, they can’t get toxoplasmosis.
- Avoid feeding your cat a raw diet: again, no infected meat consumption, no problem.
- Have another family member or friend clean out the litter box once daily. (You might already be doing that if you were averse to smells as much as I was in my first trimester!)
If you are concerned about your possible exposure risk to toxoplasmosis, be sure to speak to your own physician about testing.
Changes in the Home
There are so many changes that come with a baby. Our little lady isn’t even here yet, and our house already feels so different. Your pets are aware of these changes too. It’s important that we try to anticipate changes to our pets’ schedule and lives so that we can prepare them, because once baby is here, there will be enough to worry about.
One new item is the stroller. If your dog is like our Emmie, she gets spooked by everything from a plastic bag floating in the wind to the vacuum cleaner. She has definitely barked at other people pushing strollers. It’s important to introduce the stroller before there’s a baby in it and get the dog used to walking with the stroller. If that means you’ll be that crazy neighbor pushing around an empty stroller with your dog, just say your vet made you do it. For dogs fearful of strollers, use positive reinforcement to create a positive association with being near the stroller. (For Emmie, that means treats—and LOTS of them!) Also, remember that you should NEVER attach your dog to the stroller when cruising with baby.
The car seat is another common piece of baby equipment that you’ll want to expose your dog to. Practice getting in and out of the car with your pup. You’ll want to make sure that your dog cannot get to your baby while in the car. You can purchase a dog seat belt or have a small crate available.
Introducing Baby to Your Pets
Have a family member or friend bring home something from the hospital with the baby’s smell on it before the baby’s arrival. The day baby comes home, have everyone come in before the person holding the baby come in. Keep your pet distracted with praise and treats while the baby comes in, and try to stay calm.
Later, while the dog is leashed, allow her to gently investigate, maybe just smelling at the feet for a short while. Then give your dog lots of praise for the gentle investigation. You want to avoid punishment, instead rewarding and praising gentle calm behavior. Avoid allowing the pet to lick the baby (but a few licks at the feet is not a huge concern). And never leave baby alone with your pets, ever.
Be sure to speak with your veterinarian if you think your pet may need medication to help with the anxiety of the changes that come with a new baby. Sometimes having an anti-anxiety medication can help with the transition to this great new adventure that the whole family is starting.
For more detailed information, the ASPCA and Veterinary Partners have articles that are very helpful, and please always feel free to contact your veterinarian.
Finally, I would like to thank all my wonderful colleagues and staff here at Medical District Veterinary Clinical for their support and well wishes as my husband and I get ready to welcome our future Illini!
She’s due at the end of this month, so if all goes according to plan, I will be on maternity leave through April, with Saturday hours starting again in May, and back to full time in June. We are very excited (and a little nervous) to start this next big adventure in our family!
—Alyssa Kritzman, DVM
Marijuana Toxicity and Your Pets
![[marijuana]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2020/01/marijuana-pets.jpg) Seek Veterinary Care for Pets Exposed to Marijuana
Seek Veterinary Care for Pets Exposed to Marijuana
Now that marijuana is legal within the state of Illinois, we anticipate an increase in pet toxicities within our clinic. Over the past six years the Pet Poison Hotline has seen more than a 450% increase in cannabis toxicities across the U.S. Within Chicago and Illinois, I expect to see more pets exposed to cannabis toxicosis now that the drug is legally available. As a result of edible marijuana products, many of these cases involve co-toxicities with chocolate and/or raisins in addition to cannabis toxicity.
There are three main categories of cannabinoids. THC, commonly referred to as marijuana, is the cannabinoid that is most commonly associated with toxicity. CDB, or the non-psychogenic cannabinoid, has a much wider safety margin and is currently being researched as to its true efficacy for both pain and seizure control. While CBD appears to be very safe, there is limited science regarding safety, efficacy, and purity of products. The third form is synthetic cannabinoids, which are illegal recreational drugs in all states and cause the most severe clinical signs.
CBD Oil Cautions
While there is limited research around CBD, many pet owners and companies feel there are positive benefits of its use. I recommend using caution because there is very little control over the market and thus the purity of the products can be extremely variable. Dr. Bill Gurley looked at 25 CBD products available in Mississippi. The products were analyzed, and the results were compared to the label claim. In many cases there was no detectable CBD present and in other cases there was a much larger percentage of CBD than the label stated. One product had CBD concentration 2000% higher than the label claim.
The lack of regulation can pose a risk for pets. Additionally, there is some early research that high doses of CBD may result in hepatic toxicity and increase liver values in mice. It is unknown if similar effects are seen in cats and dogs, but many believe they may experience similar side effects. The research is conducted by Drs. Igor Koturbash and Bill Gurley at the University of Arkansas School of Public health. To read their abstract click the link below: https://publichealth.uams.edu/departmentsandunits/centers/cdsr/research/
Signs of Marijuana Toxicity
Animals exposed to any cannabinoids may experience adverse effects. Animals that have been exposed to marijuana can experience many of the signs seen in people, but the most commonly seen signs include drowsiness, depressed mentation, ataxic gait (wobbly), and urinary incontinence (dribbling urine). Less commonly pets can experience vomiting and diarrhea. In severe toxicities hyperactivity, hyperthermia, and seizures have been reported.
Pets that are exposed to synthetic cannabinoids usually have more severe effects.
Additionally, some of the most severe toxicities result from ingestion of edibles resulting in co-toxicities. If you think your pet has been exposed to marijuana, have your pet assessed immediately so appropriate steps may be taken to care for your pet. These steps may include decontamination, activated charcoal administration, and monitoring of respiratory rate, heart rate, and blood pressure. The steps will likely be different for each case, depending on the level of toxic exposure, the type of exposure, the time frame post exposure, and the clinical signs currently being experienced by the pet.
Keep Weed Out of Pet’s Reach
So the moral of the story is to keep all marijuana products out of reach of your pets and use CBD with caution. I have spoken with a lot of owners who are currently using CBD products and they have varying opinions. In some cases owners report huge improvements, but more commonly they see little to no improvement. I have not observed major side effects of CBD products in pets, but please use caution. If you ever suspect your pet is having adverse effects, please discuss with your veterinarian and have your pet examined.
Dr. Drew Sullivan
Medical Director
Tips for Traveling with Your Pet
![[dog and cat with maps and suitcases]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2019/12/mdvc-slaughter-travel-blog.jpg) As the holiday season approaches, many of you will be traveling near and far with your four-legged family members. Flying with pets has become increasingly common over the years, and as a result of the growing number of pets flying, the travel requirements for many airlines have evolved.
As the holiday season approaches, many of you will be traveling near and far with your four-legged family members. Flying with pets has become increasingly common over the years, and as a result of the growing number of pets flying, the travel requirements for many airlines have evolved.
The change in pet travel requirements can be a big surprise for many owners. I have witnessed many owners that are stressed and nervous at the final hour, trying to get everything together for their pet’s trip. The to-do list can seem endless, with many hoops to jump through. I cannot stress enough the importance of proper preparation.
Therefore, to aid in your travel plans this holiday season, and in the future, I put together some tips to help you prepare for airplane travel with your pets:
- Check the specific airline pet travel requirements
Each airline has different requirements for travel – including vaccinations, documentation filled out by the veterinarian, and carrier size. If your pet is not traveling in the cabin with you, there will most likely be additional steps to take to ensure they are ready to fly.
- If traveling internationally, research travel requirements of the destination country
For travel outside of the United States, additional planning and health care requirements may be required. I recommend checking the APHIS (Animal and Plant Health Inspection Service) Pet Travel Website to research all requirements for the country that you are traveling to. Below is the website:
https://www.aphis.usda.gov/aphis/pet-travel
You should also contact the foreign office of the country you are traveling to for more information.
There are pet travel companies that can help coordinate and organize all travel requirements and documents. This is especially helpful for international travel. In my experience, their service is extremely valuable for owners.
- Contact the Veterinarian
You have done your research, so it is time to see us! For some countries, you need to begin the process months in advance, and even when traveling domestically, a health certificate is required (often within 10 days of travel). Therefore, please plan accordingly when scheduling the visit.
I hope this is helpful! Please feel free to contact us if you have any questions about your pet’s travel plans.
Happy Holidays!
Amber Slaughter, DVM
Thanksgiving Holiday Hours 2019
Our clinic will close at 4 pm on Wednesday, Nov. 27, for the Thanksgiving holiday. We reopen at 7 am on Saturday, Nov. 30.
Wishing everyone a warm and happy holiday!
If you need emergency veterinary care while we are closed, please visit MedVet Chicago, 3123 N. Clybourn Ave., Chicago; (773) 281-7110.

![[dog near gourds]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2019/11/thanks-dog_web.jpg)