Our Blog
Holiday Bummer Blog Answers ‘What Is an Emergency?’ (and Spreads Fear-Based Cheer and Goodwill)

The sprawling earth-warming record-breaking green Christmas of 50-degree weather and rainstorms once again fills us with nostalgia at this time of year.
Ice-cold eggnog and air conditioners whir to the crash of Christmas trees being brought down by your pandemic puppy’s first attempt to eat ornaments, your Aunt’s novelty gift of “football”-scented candles exude hints of leather and burning bushy cattails, and, of course, OF COURSE, your hypothetical 7-year-old son (who seems to only like the first bite of $15 pastries) has fed the tenth hypothetical chocolate Santa to his hypothetical best-friend dog, which is now hypothetically a zombie from the amount of hypothetical grapes, coffee, ant traps, and chocolate-based gifts he has hypothetically ingested by way of one’s hypothetical son.
And with this picture painted, I bring to you again another uplifting Spirit of the Holiday bummer blog post about EMERGENCIES and fear-based cheer and goodwill.
To ER, or not to ER?
Yes, you know that this time can be stressful for some. And despite my oddly disproportionate love of the holiday season that brings a 300X increase in workload and overall Things That Need to BE DONE RIGHT NOW, I never tire of holiday puppets playing jug band music as a soundtrack to the slew of catastrophic pet events that seem to dominate my life via a 24/7 stream of strangers reaching out to me because their cousin’s cryptocurrency dealer’s previous neighbor once brought their cat to see me in 2019 for a wellness exam and they heard that I would help.
And because this is my last blog post before my departure to the ER world, I also wish you all goodbye and thanks for everything.
Dr. Brett Grossman
And the question always comes down to a form of this: My dog/cat just did something to my something and is either acting undefinably weird, is sleeping, has blood pouring out of their eyeballs, or possibly coughed once.
Should I go to the ER right now despite having to meet my Anti-Vax Uncle from North Carolina at the airport in one hour? Or can I wait until next week when I will have more time?
So what is an Emergency and when should you act? And after I say you should go to the ER, when should you actually listen to me and when should you google to find out why seizures are normal for adult dogs staring at Christmas trees?
Listen to Your Veterinarian
First, I cannot know if anything is an emergency without evaluation. If you think your cat or dog is not doing well, is suffering, or if you need evaluation by a doctor to be able to enjoy said Anti-Vax Uncle’s visit, then just go to the ER. You don’t have to be afraid. Most ERs are equipped to deal with nervous dogs, cats, and people. The wait may be long, but that’s because there are 600 people on your block alone going through the same thing right now. So just go and treat your ER staff nicely.
Second, listen to your vet. I may have some bias, but we have families, pets, and a full schedule too. We have already squeezed in 10 people this morning, so even if you only want to see a particular doctor, if we tell you to go to an ER it’s not because we don’t care. It may be because we cannot give the treatment that your pet deserves given the schedule and our brain’s load of, honestly, dying and sick patients. If Sir Puggle Wuggle may have swallowed your friend’s custom-made Run-DMC Christmas ornament and is doing fine and you want to be seen, going to ER may be the only option.
So. What Is an Emergency?
- Anything your regular trusted vet tells you is an emergency. (Don’t try to out-google-smart them to get the answer you want.)
- If your animal is in pain: Crying, screaming, cannot get comfortable.
- If your animal is non-responsive: Won’t get up, won’t wag its tail, won’t respond to things it normally responds to.
- If your animal ingested a known toxin: Anti-freeze, chocolate, rat bait, a whole bottle of CBD chews that your sweet Anti-Vax Uncle brought you and then left on the table, Tylenol, an overdose of prescribe medication such as insulin or anti-inflammatories. You can always call the ASPCA poison control hotline for advice: (888) 426-4435
- If your animal is unable to breathe correctly: Wheezing, panting, congested, is turning blue.
- If your animal is bleeding from somewhere, and it will not stop.
- If your animal is having active seizures.
- If your animal is uncontrollably anxious and you can’t figure out why.
- If your animal has a broken bone, was hit by a car, suffered an extreme trauma like burn, severe cold, attack by a dog/coyote/Anti-Vax Uncle.
- If your animal cannot go to the bathroom (not hasn’t gone to the bathroom, but is trying and cannot).
- If your animal has GI distress: Vomiting non-stop, having non-stop diarrhea, not eating for days in a row.
- And, as a general rule, if you are freaking out because something is not right and you know your pet better than anyone else and you just know something is wrong. (This is valid.)
No One Likes a Holiday Tragedy
In these cases, and other select cases I didn’t think to mention, you can call and ask. But just plan on going to the ER.
I say this while acknowledging that not everyone can afford a visit to the ER, but don’t fear a $10,000 bill. Some things are the same price as a visit with us. Making a dog vomit up a Run-DMC ornament won’t be a life-altering expense, but waiting for the Run-DMC ornament to pass, it getting stuck, and needing a life-saving surgery in 2 days may be. It’s Like That and It’s Tricky.
I also realize that if you are home alone with a child at 2 am, you cannot always run somewhere and take care of it, but, sometimes, the alternative is to explain to an awake child something worse about Sir Puggle Wuggle, and then we are entering every Holiday Tragedy movie about angels in heaven, and I don’t like these movies at all. Nope.
What Isn’t an Emergency?
Note: Do not avoid going to the ER because of this list and blame me for it, but these are common things people call about that don’t require immediate attention.
Your animal is generally doing alright, happy and alert, but:
- Your animal hasn’t eaten today.
- Your animal had some loose stool (even a little blood in it).
- Your animal vomited twice this month.
- You think your animal may be losing weight.
- Your animal seems to be favoring one leg but is not in terrible pain.
- Your animal sneezed or coughed.
- Your animal has some discharge from the nose or eyes.
- Your animal didn’t go to the bathroom today.
- Your animal is scratching, you saw fleas, you found a tick and got it off.
- You saw some worms in your animal’s feces.
- Your friend/uncle’s dog just died of cancer and you are worried that your animal has it.
There are countless more. I’m not saying that these things aren’t worthy of being addressed. And of course if any of these things causes discomfort, pain, or anxiety on your part, going to the ER is not wrong. I’m just saying these things do not require immediate attention on Christmas Eve (or as we one-eighth Jewish Canadians refer to as “Justin Trudeau’s birthday eve”).
My Hopes and Wishes for You
I can totally follow a scenario where you keep your animal at home and monitor and one of these non-emergencies turns into one. But for now, there are plenty of OTC fixes that we can recommend to help before an ER visit is needed.
So, I hope all your holiday plans go seamlessly well without trauma or tragedy. I hope your new year is safe and fun.
And because this is my last blog post before my departure to the ER world, I also wish you all goodbye and thanks for everything.
Vaccinate, stay safe, and please read this book and become the tree you deserve to be.
Brett Grossman, DVM
Salty Paws Make Salty Dogs

Rock Salt Is the Real Culprit
There comes a point at the end of every year when you can no longer just grab the leash and causally head out for a walk with your dog. (That is, unless you have a Bernese mountain dog like my brother’s dog, Ruby, who would live in the snow if she could.)
Instead, you have to determine how many layers of clothing you and your dog need to go for a walk. I’ve been doing this dance for years with Emmie. Eventually she complies, thankfully. But, just once, I wish she would remember that when we don’t put the booties on and there is salt out, she ends up crying out and her paws hurt.
As cold as our Chicago winters are, there are really only a few days in any calendar year where it is so cold you have to truly worry about a dog’s paws. The real culprit that is causing dogs to lift up their paws and look at you like they’re auditioning for an ASPCA commercial is the rock salt. I’ve definitely had to carry Emmie a few hundred feet through a heavily salted sidewalk stretch when we were caught off guard.
So here are two ways to help protect your pet’s paws, plus what to do if you forget:
Booties
Yes, they are annoying to put on. Yes, they can sometimes fall off. And yes, most dogs don’t like putting them on. But booties are by far the best way to protect your dog’s paws, and when she’s outside she’s much happier.
The key is to find a brand that fits your dog well. Put in the extra effort to measure the size of your dog’s paws for best fit and look for waterproof options, if they are in your budget.
I’m a fan of Muttluks. They have a measuring guide to help ensure the best fit. Remember: Never use a rubber band or any other band that can be constricting to hold up the booties.
Balms
These can be used to try to prevent ice balls from forming between the toes. Balms also help keep small amounts of salt from bothering their paws. The base ingredient for most of these balms is beeswax, but sometimes you can use coconut oil as well.
The most common brand I see is called Musher’s Secret, though a lot of other brands are out there. The upside is that most of these can be licked or ingested with no concerns. The downside is that they tend not to work as well as booties.
Remedies
If you are like me, sometimes you forget. (Or, TBH, are too lazy and depressed about how dark it is at 6:30 in the morning. Even after we go back to standard time, ugh! Which if any of you have a toddler like me, does not mean an extra hour of sleep!)
When you forget and your dog gets salt on her paws, rinse them off with cool water once you’re home. A warm water Epsom salt soak for 5 to 10 minutes will usually fix the problem if her paws are still irritated after everyone has warmed up from the outing. If the paws are still irritated or seem painful after a soak, give us a call.
What Food Is Best for Your Dog or Cat?

This is a question and a discussion that I have with clients daily. And to be honest, it’s a very difficult question to answer. I am going to give you a few tips on how to pick out a food that is best suited for your dog or cat.

Life Stages
I recommend feeding a food based on the life stage of your pet. The four life stages include growth, young adult, mature adult and senior. The below picture helps illustrate the life stages of cats. Canine life stages are pretty similar, but with more variation due to the vast size difference we see in the canine species. The growth life stage is typically done by 6-12 months of age. For cats the growth phase is typically finished by 6-10 months of age and I recommend transitioning to adult food around that time. If you have a puppy or kitten it is very important for proper growth and development to feed a puppy or kitten food. In the same manner as your pet is aging feeding a senior diet is important as they have different nutrient profiles.
You may ask what about an “All Life Stages” dog or cat food. For a company to market their food as “All Life Stages” the food must meet the nutritional requirements for all life stages. Therefore, most of these foods are formulated as a puppy/kitten food because puppies and kittens have the highest nutritional requirements of the four life stages. These foods can be good foods and well balanced, but they typically have a high caloric density. Therefore, in my experience, dogs are more likely to become overweight than if they were fed some other diets.
Medical Conditions
Does your pet have any health conditions that require a special diet? Prescription diets can play a vital role in management of many health conditions, including kidney disease, diabetes, obesity, allergies, and feline lower urinary tract disease.
If your pet suffers from a medical condition, diet can manage and help many conditions, so I always recommend considering a prescription diet if you pet has one of the above conditions.
More Expensive Does Not Mean Better
Many pet food companies are great at marketing but might not be as good at formulating diets. You can always look for the Nutritional Advocacy AFFCO (Association of American Feed Control Officials) Statement on each bag or can of food. These statements will tell you if the food has been through a food trial or formulated to meet particular feeding guidelines. The ingredient list should also list all ingredients in decreasing amounts by weight.
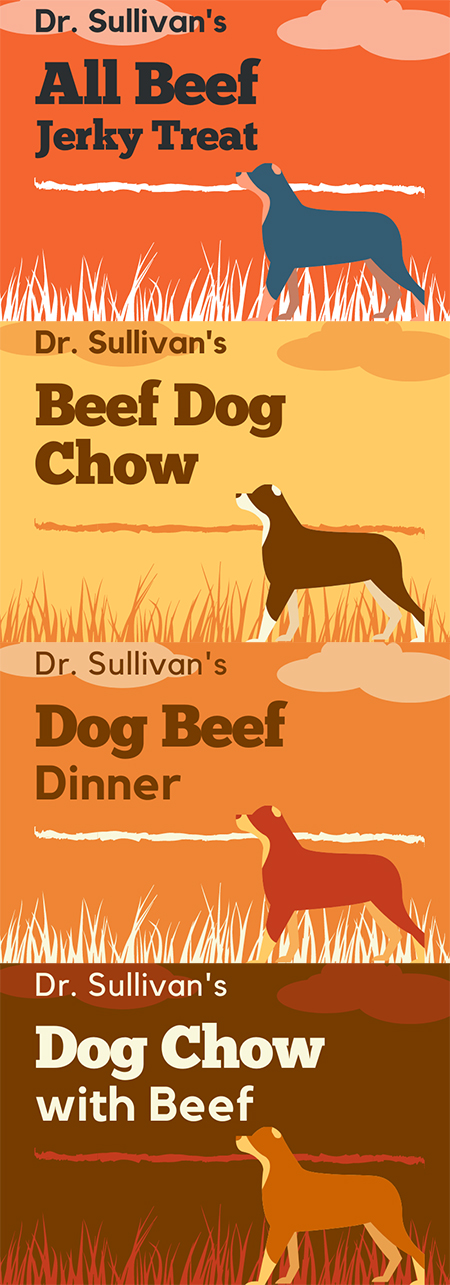
Labels are very confusing and often misleading to consumers. For example, if I made up a food with the following labels, the variation in ingredients can be drastic.
- If the term “All” is used, then the ingredient must make up 100% of product minus preservatives and water. So, this treat would be 100% beef
- If the listed ingredient is used, then the ingredient must make up 95% of product minus water. So, this Beef Dog Chow would be 95% beef on a dry matter basis.
- If the term “dinner,” “platter,” or “recipe” is used, then the ingredient must make up only 25% of product. So, this Beef Dinner is likely only 25% beef.
- If the term “with” is used, then the ingredient must make up only 5% of product. So, this Dog Chow with Beef is likely only 5% beef.
I hope this illustration helps demonstrate how confusing pet food labels can be to both consumers and veterinarians. I recommend visiting the AAFCO website if you want to be better educated about what’s in your pet’s food.
Say No to ‘Grain Free’
Does my pet need grain-free food? The answer is NO. There little to no research showing the true benefit of grain-free food. In fact, grain-free food has been shown to cause heart disease in some dogs. The exact cause is still being researched. Visit this site for more information. https://www.fda.gov/animal-veterinary/animal-health-literacy/questions-answers-fdas-work-potential-causes-non-hereditary-dcm-dogs
What About Raw Food?
Some dogs do really well on raw food, but I do not recommend it. That’s because I see too many owners who try to feed raw but who are not feeding a balanced diet because they are solely feeding raw meat and limited other nutrients.
In the wild canines and felines will consume entire animals. Eating meat, skin, ingesta, organs, and bone makes up a balanced diet.
Raw can be balanced and can be a good diet for some animals, but there is also a public health risk with feeding these diets. This is a statement from the CDC:
“Germs like Salmonella and Listeria bacteria have been found in raw pet food, even packaged ones in stores. These germs can make your pet sick. Your family can also get sick by handling the food or by taking care of your pet.”
Centers for Disease Control and Prevention
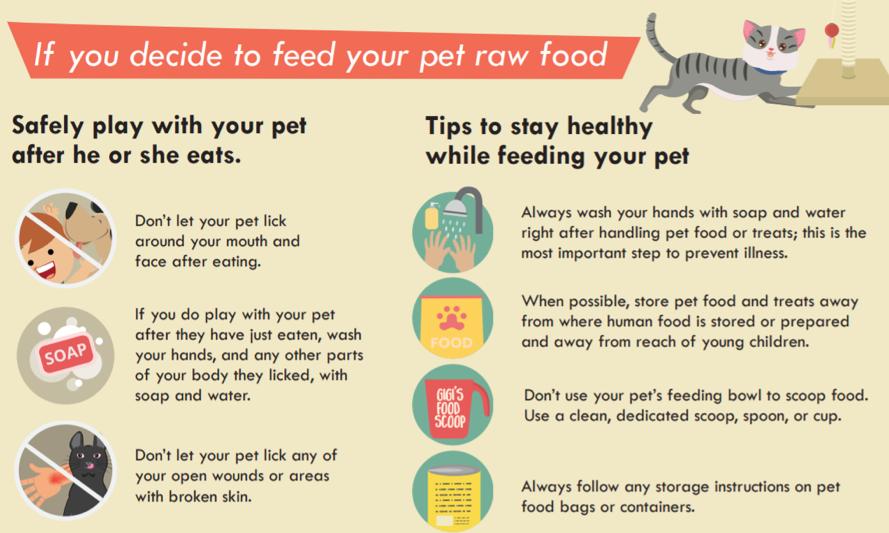
Therefore, if there are young children or anyone who is immune-compromised in your house, I highly advise against feed raw pet foods.
Each Pet Is Different
I hope this information has been helpful and informative. I recommend discussing your pet’s daily calorie needs with your veterinarian as each pet is different, just like people. Two people that have ideal weights of 180 pounds may be able to eat very different diets to maintain their weight, and the same goes for cats and dogs. All 10-pound cats do not need the same daily calories.
The recommendations on the bag or can of food should only be a guide. Some animals may need more calories, but most will need less than the recommended amount to maintain an ideal weight. And always remember to factor in all treats and table scraps into their daily calories. Most pets are overweight these days.
—Dr. Drew Sullivan
Fear Free Practices for Furry Friends

For many people, the doctor’s office can be a scary place. So it is no surprise that many pets view going to the vet with a similar fear.
Our clinic truly believes in Fear Free practices. Our goal is to limit your pet’s stress and fear and make visits with us as pleasant as possible. There are various ways that we do this, which I would like to share with you.
Treats, Teats, and More Treats!
During your pet’s visit you will notice that we like to offer treats. We have biscuits, cheese, peanut butter – like a candy store for dogs and cats! This is not only because we think your pet is adorable and we want to spoil them, but this is also a main way we like to bond with them.
Imagine if you are at the doctor and you are anxiously waiting, and then the doctor walks in and immediately offers you your favorite treat (for me, that would be some delicious baked goods) and socializes with you. You would likely feel much calmer and connected to them. This is the equivalent of what we do with your pets.
Although we have lots of treats, if you have a dog or cat that is pickier with food, please feel free to bring whatever your pet likes best. This is not uncommon, as I have seen many patients that would eat only one food.
We encourage owners to offer treats as well during visits to help make the entire experience as positive as possible. We joke that visits go best when our patients come hungry, so you may want to consider bringing your pet to see us with an empty stomach so there is plenty of space for treats!
Getting on Their Level
We want our patients to feel comfortable, so we often will sit on the ground with them. We hope that by sitting on their level they feel less intimidated and fearful, and that they see us as their “friend.” I have noticed that when I sit on the ground and spend time in the room before even beginning my exam, my patients generally seem more at ease.
Please do not feel obligated to sit with us, but if you would like to you are totally welcome!
Limit Stress from Other Pets
Many cats never leave the home except to go to the vet. They may be stressed by traveling before they even arrive.
The smells and sounds of dogs can be very scary for them, too, which is why we recently created a separate feline waiting room and exam rooms. We use all separate supplies, have tasty treats and fun toys, and have nice feline-friendly smells. In the months since we have started using this new space, I have noticed that cats overall seem much calmer and happier.
Dogs can be become upset from other pets as well. Some of the sweetest and most affectionate dogs that I have met do not get along well with other dogs. Being around other dogs is stressful for them. I personally have a dog-reactive dog, and while she loves people, other dogs make her highly anxious.
To reduce this anxiety, we have multiple tactics, such as choosing specific exam rooms and trying to limit time in the clinic and exam room, when other pets are a trigger for the patient. We also perform exams outside in an isolated area if needed.
Fear Free for Your Pet
Please let us know if your pet is reactive with other pets, or there are any other behavioral concerns, and we will work with you to formulate a plan for their visits.
I hope you can see how much we at Medical District Veterinary Clinic truly care about our amazing patients! We look forward to continuing to make their time with us as fun and enjoyable and fear free as possible!
Amber Slaughter, DVM
Dr. Grossman Reprises His Anal Sac Primer

Well, it’s been 17 months of a global pandemic and it’s the middle of a hot (UN Climate report) summer. Though much has changed since March of 2018, dogs’ anal sac health dramatically has not. Partly because I’m tired, and partly because I answer questions about this about 20 times a day, I wanted to re-run a classic of yesteryear that takes us back to times more innocent, when a postage stamp only cost 50 cents and kids couldn’t get enough of this “texting” craze. Enjoy.
Most of us in the veterinary field face a horrible dilemma. The majority of our days are filled with details and particulars that are deemed rather unfit for discussion at the dinner table, any social gathering, and anywhere outside the professional confines of the clinic. It’s always fun to talk puppies and kittens, but a great deal of what we do during the day revolve around bodily fluids (blood, feces, urine, vomit), wounds, parasites, and the selected greatest and grossest hits of infection and disease.
Anything interesting happen at work today? Yes. Most of it was gross.
So, I’d like to discuss the grossest of all things for one moment. Please feel free to put away your chocolate custard, beef stew, and bean soup, for one moment, while we explore dog and cat anal sac disease.
Cats and dogs have anal sacs located near the periphery of the anus. These sacs excrete a liquid, often when animals defecate, that mixes into their stool and gives forth a particular and specific smell akin to a garbage bag filled with a rotting animal that has been soaked in plague juice.
At times, though, the ducts that excrete the anal sac fluid can become blocked, forcing the sacs to become enlarged, uncomfortable, swollen, and irritated. Sometimes these sacs can become so blocked that they burst forth with a mixture of all of the aforementioned dinner-party unmentionables in one fell swoop. Other times they slowly leak out at convenient times and places such as Sunday morning at 5:13 a.m. on your pillow next to your head. Often, they don’t do anything but get bigger and more uncomfortable. There are times when severe stress and discomfort can cause animals to release their anal sacs all over (seemingly) everywhere in the world.
Owners complain about their dogs and cats “scooting” their back ends over the ground or that their pets are licking their back end obsessively. The clinical signs may be more vague and scary, especially for older animals who have not ever had this problem. We may find out animals straining to defecate (as the sacs block the exit of the anus), walking stiffly, uncomfortable, not interested in eating, and, in extreme cases, vomiting. I’ve seen some dogs become so affected that they scream in pain when touched and refuse to move. I’ve seen some cats stop eating or moving and refuse to go into the litter box.
Why does this happen? you ask (while not at the dinner table). There are a few common reasons:
• Anatomical irregularities that are uncontrollable: Some dogs and cats, for whatever reason, just don’t seem to have anal sacs or anal sac ducts in the right position to allow for easy release. We have seen puppies whose anal sacs fill up monthly and need help.
• An extended period when the animal’s feces are soft and unable to naturally press on the sacs to express them: When animals have parasites (such as Giardia) or chronic diarrhea due to dietary issues or underlying illnesses, we often are not thinking that during the whole of this period, their anal sacs are (metaphorically) laughing with power as they grow bigger.
• Infiltrative disease (such as cancer): This is not very common, though it can occur. The anal sacs become diseased and cancerous. It can happen in any dog, but one tends to see this more in spaniel breeds. It does not have a good prognosis, but this condition is rare. Very rare.
• Animals, especially as they get older, learn different postures to deal with changes in the body. I have seen so many cats and dogs with untreated back pain that have to posture differently to defecate, and because of this, do not seem to express their anal sacs with the same proud efficiency that they once did. As the anal sacs get worse, they become even more uncomfortable, the animals defecate less, develop chronic soft stool, and this glorious cycle continues until you have a cat or dog that is constipated and has horribly painful anal sacs.
What can you do about it?
First, express the anal sacs. This is not something one should just try at home. I am speaking for all citizens of earth, in general, by saying that you should not do this in your kitchen before the family wakes up. Partly, because the smells of putrid sub-par day-old fish byproduct mixed with armpits and feces will probably wake them up, but also I wonder if this aspect of your relationship with your pet is one you really want to explore. While some people do learn to do this at home with their animals, I personally will not do it at home on my animals. But it is possible.
Alternatively, we can express your animal’s anal sacs so you don’t have to watch, smell, see, and, in some tragic cases, taste. We have safe zones in the clinic where no one walks for fear of spraying anal sacs. Some groomers do this for you, but few do them to completion. Ask your groomer before you assume, and talk with us about how soon you should come back for a recheck. Sometimes the anal sacs can be so full and painful that sedation may be required.
Second, animals may need additional treatment, such as antibiotics or anti-inflammatories. Most bad cases of anal sacculits, anal sac impaction, or anal sac abscesses need medication and aggressive rechecks before they are not painful or affected. It’s not generally the case that medications alone will work.
Third, we must remove the cause. Are allergies causing chronic licking, which is causing the anal sacs to be inflamed? Is your animal’s diet not allowing for a normal stool texture? Do you need to add fiber to the diet? Is your dog anxious, and this anxiety manifests in back-end licking? Are there intestinal parasites present? Is there infiltrative disease? Is there a chronic infection? Is there another animal in the house that is over-grooming the affected animal? We need to fix this.
Fourth, sometimes the anal sacs need to be removed. It’s not a cheap therapy, and it is surgery. But sometimes after coming into the clinic every two weeks and having anal sac disease a constant part of their lives, some owners elect to remove them.
As a final note, most dog owners know or have heard of anal sac issues, but most cat people are thinking that this is not applicable. This problem affects many mammals. So I’m sorry to say that even the sweetest of felines has the foulest of anal sac scents. I’ve had a run, lately, of seemingly ill cats who magically became “new” cats after their anal sacs were expressed. And, for those who play with the skunks, beavers, and opossums of your neighborhood, though I’m sure you have more on your mind, also be aware. Humans have them too, but I will let you and your loved ones google that on your own on your non-work computer.
Read things from Canada, do anything related to Canada, enjoy the summer weather noticed when opening the windows after the scent of your animal’s anal sacs permeate the walls of your Chicago apartment.
Brett Grossman, DVM
Medical District Veterinary Clinic
Pets Put on Pandemic Pounds Too

Now that the end of the pandemic seems to be in sight, we are starting to think about returning to normal activities, our pets included. Getting out more and stretching out legs, we may notice that there’s a little more of our pets than there was in 2019, in a very physical sense.
At the Medical District Veterinary Clinic, we have seen a lot of pets gain weight over the last year as routines and activities changed. I know my dog, Emmie, has definitely got a little thicker. (Having a toddler in the house hasn’t helped Emmie’s weight, either.)
When it comes to pets’ weight loss and healthy weight maintenance, you should know that exercise helps, but what they consume is often more important. That doesn’t mean you shouldn’t get out there and go for walks, hikes, or trips to the beach with your dog. It’s just that how much you put in their food bowl will help more.
Also remember not to discount the little things. Small snacks add up, especially when you weigh only 11 pounds and need only 225 calories a day. That’s a healthy serving of peanut butter! That little extra snack may not seem like much, but it’s a lot for your pet. Remember that the recommendations on your pet’s food bag assumes that they are getting no other calories.
If you feel like you’re really calorie counting and the scale is going nowhere for your little fluffy, let us know. Some animals need a little extra help in the form of a prescription diet. In the same way that some people have a harder time losing weight, so can pets, and a special diet may help.
Finally, if your dog or cat is losing weight and you haven’t changed their diet or exercise, let us know. Weight loss isn’t always a good thing, and we will make sure they are okay.
Enjoy the rest of summer!
Alyssa Kritzman, DVM
Tips for Parenting a Puppy
![[Dr. Sullivan's puppy, Winnie]](https://www.medicaldistrictvet.com/blog/wp-content/uploads/2021/06/winnie.jpg)
Life as a new pet parent can be challenging, and to be honest, you never really know what to expect. After losing Oskee, our dog of 14 years, last fall, I knew our family would get a new dog, but we just didn’t know when. We were not in any rush, but over the past few months, we were discussing it more and more.
This past month we adopted a puppy from a rescue in Central Illinois called Hudson’s Halfway Home. I had the privilege of working with this rescue group before moving to Chicago, and they do amazing work. Our family was lucky enough to adopt a 6-month-old puppy, and she has been a great addition to our family.
Even though I see puppies daily, it had been more than 15 years since I had a puppy at home, so I had a lot to think about before bringing Winnie into our family. Here is my list of ways you can help set a puppy up for success.
Routine
Most important is creating consistency among all family members to avoid confusion for new puppies. Having a routine that everyone follows around housetraining, feeding, basic commands, and so on will help your new dog catch on quickly.
Housetraining
When it comes to housetraining, it is very important to be proactive early on. Puppies initially will not ask to go outside to go to the bathroom. Anticipating when they may need to go and then providing a small reward once they go outside is key. Additionally, do not confuse puppies by trying to teach them both potty pads and grass early on. I always tell owners if your goal is to train to go to the bathroom outside, that should be started from Day 1. After they are puppy pad trained, they can still be trained to go outside, but it may be more challenging.
Consistent diet
Puppies commonly have intestinal parasites and are also known for eating/chewing on everything. Keeping puppies on a consistent diet will help keep their bowel movements regular and predictable. Feeding an overabundance of treats and/or human table scraps will likely lead to soft stool/diarrhea. When puppies have diarrhea, the frequency of defecation increases, so accidents inside are common, further delaying potty training. Not to mention that a poor diet could make puppies very sick. I always say avoid the human food. It is not a good habit to start at such a young age.
House safety
Be sure you puppy-proof your house and have limitations for your new puppy. I highly recommend crate training. Crates are not to be used as a source of punishment, but a place where puppies feel safe and secure. The training may take time, and you may need to sleep next to the crate initially, but once puppies realize it is their safe place, it is wonderful. Having a dog crate trained also keeps dogs safe when you are away. If crate training is not for you and your puppy, then using baby gates to create boundaries can be used similarly. In addition to boundaries, make sure all garbage cans have lids or are in cabinets. Be sure electrical cords are placed where puppies can’t chew them. Keep all cleaning products away from the puppy. Puppies love socks, so use caution to prevent your puppy from eating your socks.
Preventive care
It is very important to take your new puppy to the vet as soon as possible for an overall health check and vaccines, if needed. Typically, puppies receive vaccines at 8, 12, and 16 weeks of age. Additionally, puppies should have an intestinal parasite screen for worms (very common in puppies) and need to be started on heartworm, flea, and tick prevention as young as 6 to 8 weeks of age.
Socialization
It is very important to socialize puppies with both dogs and people. Puppies mature so quickly that it is important to start socialization very early on.
Insurance
If you are considering insurance, the best time to purchase is when you have a puppy with, hopefully, no pre-existing problems. Once a problem occurs, most companies will consider it pre-existing and insurance will not cover treatment of that problem the remainder of that pet’s life (allergies and ear infections, for example). There are many insurance companies, so to find one that’s right for you consider whether you are looking for coverage for accidents and illness or full coverage that includes wellness/preventive care.
Over the past three weeks, our family has made changes to our routines to accommodate Winnie. She is adjusting well and, luckily, our house is somewhat puppy-proof because it is somewhat kid-proof (minus all the kids’ toys).
We are crate training her, and she is doing great. She loves her crate and goes in willingly at bedtime. During the day, she prefers never to go in, but when we leave the house, she does great in her crate. When we are home, she goes outside to pee every few hours, and she can make it through the night without an accident. So overall, housetraining is going very well, though there have been a few accidents.
We are both trying to figure each other out. Since she had lived in a kennel setting for 4 months, the grass and leash walking were brand new to her. Now that she is catching on and is gaining confidence outside, she is doing well. She still does not alert us when she needs to go out, so we try to stay proactive in telling her it’s time to go “potty.” With a continued consistent routine, I’m confident we will be accident-free in a short time.
Like many of you, we are thrilled to have a new dog in our home. We love having Winnie in our family. Start early and stay consistent to set your puppy or new dog up for success.
Dr. Drew Sullivan, Medical Director
Make Room for Kitty

The spring is one of my favorite times of the year. Not only do I look forward to the beautiful weather, but I also look forward to seeing lots of adorable, newly adopted kittens. I can’t help but smile from ear to ear whenever I see them! I have been saying for months that I have kitten fever. Every day it is getting more difficult not to adopt one of my own.
Next month is the height of “kitten season.” It’s when litter after litter of kittens are born, taken to shelters and rescues, and in need of new homes. Unfortunately, there are far more pets than available homes, which further adds to pet overpopulation. American Humane celebrates Adopt-A-Cat Month each June to bring awareness to this situation and in hopes of encouraging more people to adopt cats in need of a loving home.
The pandemic has made the operations of shelters and adoptions more challenging, which makes Adopt-A-Cat Month even more important. While many people have already welcomed new four-legged family members into their families, there are still many precious and loving cats in need of a forever home. To find your forever feline, check out the websites of shelters and rescues and visit to see them in person. Be prepared to be overwhelmed by the cuteness overload, and potentially leave with multiple cats!
To help with this process, there are many resources available to help you. Many organizations provide information to guide you through this process. For example, American Humane provides literature on their website including A Cat Adoption Checklist and Introducing Cats (And Dogs) to Cats. You can also contact us if you have any questions regarding adoption. We will do whatever we can to help you find the right cat for you!
If you are unable to adopt, there are other ways to help the many pets in need. Donations (such as monetary gifts and food)can be made to local shelters and rescues. Volunteer opportunities are often available.
Adopt-A-Cat Month is almost here, so you have plenty of time to find your purrfect feline companion!
Amber Slaughter, DVM
Photo from our Instagram account.
Seizures to Shining Seizures

Oh, the nostalgia of COVID springs past. The smell of fresh crocus buds mixed with a new pandemic mask is one that evokes awakening. The freshness of April baseball overlapping with the anxiety of crowded super-spreader events, weddings, and birthday parties with only limited mortalities makes the body and brain feel young again. Socially distant first dates are in the air and all the Spring kids playing Legos together over Zoom brings back the hope squashed by the constraints of Winter kids playing Legos together over Zoom just weeks ago. The dogs and cats can feel the weather changing and with it, ramp up their dog and cat A-game. And with that, I end my introductory ramblings and segue, quite unnaturally, into a discussion regarding … your cats’ and dogs’ general neurologic behavior.
There’s This Weird Thing that Happens…
As always the bearer of angst-inducing theoretical scenarios, I would like to evoke a scene that is relayed to me often that goes like this. A dog is doing generally well. No real issues. She is eating and drinking fine, seems to be getting along with the new dog, loves to take walks, yes, there are no issues. But [hesitates for a moment], there’s this weird thing that happens every so often, I am told, and it’s probably nothing but she seems to just stare off into space every once in a while, acting like she’s not there. Then she stops, licks her leg for a few minutes, and then seems to come to and then there’s nothing wrong.
The cat version is usually something similar but often involves chasing a fly (or dust) and then twitching for a bit. I ask how long it’s been going on and often the answer is vague, like she has always done odd things like that but we thought it was just a thing, like when she goes to sleep and twitches and chases bunnies in her dreams, and sometimes whimpers… So it’s been going on for years, but it seems to be getting worse.
The Movie Version of Seizures
I think when people think of dogs and cats having seizures, they usually evoke the classic grand mal seizure like one you’d see a person have in a movie, or if you know humans with epilepsy, in real life. This big seizure in dogs and cats usually presents with them seeming off for a bit, maybe scared and hiding under the bed or in the closet for a few minutes with dilated eyes and hearts beating fast. Then the seizure will hit causing their front legs to go stiff and stick out. Their back legs paddle, their eyes can start twitching back and forth, and often they vomit, defecate, or urinate. Then comes the post-seizure time frame where they slowly come out of it and seem exhausted and not themselves for a few hours.
This would be the seizure most likely to be portrayed in the Lifetime Movie Network’s scandalous romantic thriller about a single mom/widower with a heart of gold who adopts a dog from the local church auction and then gets more than she bargained for when the dog’s neurologic activity comes between her and her rebellious daughter’s new boyfriend [screenplay pending].
Abnormal neurologic behavior is very far-ranging and sometimes we see cats and dogs act like both of the above examples and sometimes it’s even vaguer or weirder. With hopes that I am not inciting a mob of people calling with thoughts that their animals are having seizures, I will say that seizures often are retroactively understood to be seizures after they progress.
What Is a Seizure?
I’m sure you’ve heard the term “seizure,” but it’s important to know what this means. Here’s a simplified explanation: The brain is constantly activating and suppressing parts of the body through, essentially, electrical and chemical conduction. A seizure is an abnormal event where the brain is essentially not able to control its firing. It loses control of all the carefully metered out activity of the body.
Seizures can be caused by many things, and it’s important to remember that often the cause does not have to be as scary as one first assumes, especially if an animal is otherwise doing well.
Diagnosing Epilepsy
If a dog or cat is not particularly young or old, let’s just say 2 to 9 years old, the first thought is idiopathic epilepsy. This is just a way of saying, to be simpler than I like or actually have ever been, that there is no real reason or cause for the seizure.
We usually get to this diagnosis by two means. The first option is that we examine the animal and perform complete blood work to rule out metabolic and endocrine causes of seizures (like anemia, abnormal electrolytes, etc.). I usually will also focus on the heart to make sure that abnormal cardiovascular or blood pressure activity is not causing events that look like seizures. If all is normal, we monitor and see if the seizures continue while not really affecting a dog’s or cat’s life in a significant way. Sometimes we add anti-seizure medications (which are generally cheap and safe) if things are progressing. If enough time goes by and things seem controlled (with or without medications), it’s most likely epilepsy. Sometimes we have no options other than to go this direction due to limited finances or temperament of the animal.
The second option is more expensive and thorough. This would require an animal to see a boarded neurologist at a specialty hospital and most often have advanced imaging and diagnostics performed, such as an MRI and cerebral spinal fluid tap under anesthesia. I usually would have an echocardiogram of the heart performed for the reasons explained above. If there is no other cause of seizures found, we call it epilepsy, and the management is similar to option 1: monitor and start anti-seizure medications if things are getting worse.
I want to be clear, though, that seizures are serious, regardless of whether they are vague and mild or serious and dramatic. Every seizure has the potential to cause brain damage, and every seizure can be one that is life altering and even fatal. That is why doing a work-up for animals suffering from seizures is important and why we always want to rule out the other things before presuming that this is “just” epilepsy. It may not always be an emergency, but we should always see animals who are having abnormal neurologic events.
Other Causes of Seizures
And then what is it if it isn’t epilepsy? Besides being a repulsive sentence to say aloud, it also is answered by a conversation that everyone wants to avoid.
The first thing that everyone is fearful of, especially if an animal is older, is that seizures are being caused by a brain tumor. Though this is possible, there are other things about which to worry such as liver or kidney dysfunction, low blood sugar, anemia, high or low calcium, magnesium, potassium, chloride, congenital malformations of the brain, trauma, toxins, infections (viral, fungal, bacterial), diseases caused by tick bites, parasites that go to the brain, immune-mediated causes, and in some dogs we see degenerative causes that sometimes can cause our pets to act “senile.”
Unfortunately, in many cases, dogs and cats that are having seizures can be thought to have epilepsy or, at least all of the above are presumed to not be occurring. Later we discover one of these causes, like cancer, had been hiding without detection. If a cat or dog is presumed to not be suffering from all of the above and is diagnosed with epilepsy, the proper course of treatment is often, again, just to monitor or start anti-seizure medications, but if it is not working, sometimes rescue drugs like steroids are tried.
Serious But Often Very Treatable
With fear of ending on a bad note, I want to emphasize that seizures are serious, definitely scary to see, vague and can manifest in a wide-array of abnormal behavior, but often very treatable and controllable. Some dogs, though, just do weird things for no reason. My dog loses his mind whenever he sees a black bag, either on the ground or blowing in the wind, and his behavior is probably insane enough to be viewed as abnormal by most people, but he’s just crazy.
Some dogs and cats just do weird things, and this is not reason to treat your dog for a neurologic event. So let us know if you have questions and enjoy the remainder of your pandemic.
Wear your masks, read your books: https://www.bookcellarinc.com/book/9781501160349
Brett Grossman, DVM
Medical District Veterinary Clinic
Photo by Sandra Seitamaa on Unsplash
March Vaxness?

Right now with the pandemic, I don’t think a day goes by when I’m not thinking about vaccines. Granted, a big part of my job is vaccinating your furry family members to help keep them healthy and maintain their legal status, but with most of us having “Moderna/Pfizer versus Johnson & Johnson” or “one- or two-shot protocols” swirling in our head, I’m hoping to review a little bit about vaccines and their importance while I take a break from working on my NCAA bracket.
What Is a Vaccine?
I’m sure this is common knowledge at this point, but as a reminder, a vaccine is a composite of either a dead or modified-live version of a virus or bacteria that you expose the body to so the immune system to be able to quickly build a response if or when exposed to the actual virus or bacteria in the future. (We will not worry about the newer mRNA vaccines, as at this time the veterinary field does not use them.) Using a sports analogy, you can think about vaccines as giving the immune system a little practice with a disease, so it will be ready for game day.
When Do You Booster Vaccines?
In order for a vaccine to work, the immune system needs enough exposure to build up long-term immunity. That means, when the body is exposed, it not only remembers the disease, but can build a defense quickly, before the disease causes significant illness. Sometimes you need more than one practice session to master that layup; it’s the same with the immune system. Some immune systems need more practice than others. This mostly pertains to puppies and kittens: their immune systems are less developed, so they require more practice than an older more “skilled” immune system.
Why Do Some Vaccines Last Longer Than Others?
It can get a little confusing to know how long each vaccine last for. Some vaccines, such as canine and feline distemper, can provide immunity for up to 3 years in most adult pets. Others (e.g., leptospirosis and feline leukemia) need boosters every year to maintain adequate immunity. This is because the immune system is better at remembering certain diseases than others. Some people will never forget how to shoot a free throw, but it will probably take a lot more practice to maintain that hook shot.
What Vaccines Should My Pet Have?
Ultimately, you should discuss this question with your vet. Recommendations will vary based on your pet’s lifestyle and geographical location. Here is what we currently recommend for the average dog and cat that live in Chicago:
Dogs: DAPP (Distemper virus, Adenovirus, Parvovirus, and Parainfluenza virus), Leptospirosis, Bordetella, and Rabies
Cats (indoor only): FVRCP (Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia) and Rabies
When they are current on these vaccines, your dogs’ and cats’ immune systems will be ready to fight and win on the big game day.
Let’s hope our Illini are ready to do the same! I-L-L
Alyssa Kritzman, DVM
Photos by Fred Zwicky, © Board of Trustees of the University of Illinois, and Charles Deluvio on Unsplash
