Our Blog
Vaccines in Dogs and Cats / Vacunas en Perros y Gatos

“Prevention is cheaper than treatment.” A quote that I will forever remember from Dr. Vinu, a primary care veterinarian I worked for during my undergraduate studies at the University of Illinois-Chicago.
Vaccines are very critical in cats and dogs, and the vaccine series are started at a very young age. Some vaccines even need to be boosted in order for the pet to reach adequate immunity.
There are many different vaccines in cats and dogs. Some vaccines are core vaccines, meaning that they are recommended in every patient, and some are considered lifestyle vaccines, meaning that it depends on what your pet does.
Is your dog frequently boarded at a boarding facility or often goes to grooming, where they might be surrounded by many other dogs? Does your dog go to forest preserves or on camping trips where they can be exposed to ticks? Is your cat a strictly indoor cat or an indoor/outdoor cat?
All of those are great questions that are usually asked at the beginning of your annual wellness exam. Yes, we may ask many, many questions during your pet’s wellness exam, but we are putting the puzzle pieces together to recommend the best vaccine schedule for your pet.
Rabies Vaccine in Dogs AND Cats
Having your pet vaccinated for rabies is required by law. It is recommended that the canine and feline rabies vaccine be administered at 4 months of age. However, it is sometimes given earlier in a shelter setting. The first rabies vaccine is usually a 1-year vaccine, while the following year your pet can get either the 1-year or 3-year vaccine.
Rabies is transmitted via bite wounds, usually by wildlife like skunks, bats, racoons, and foxes. The virus attaches to local muscle cells, then penetrates local nerves and ascends to the brain.
There is no reliable effective treatment for rabies. Infection usually results in death of the animal. Once clinical signs are present, death can occur within 10 days.
If your pet bites another animal or human and is not up to date on their rabies vaccine, depending on their vaccine history, they might have to be confined and observed at a veterinary facility for 10 days. If the animal shows any symptoms or there is suspicion that the pet might have rabies, their brain tissue must be submitted for sampling. This means that they must be humanely euthanized for tissue submission.
Regulations can vary by state or county, so it is important to keep up with current regulations. Visit rabiesaware.org for more information regarding regulations in your area. Ultimately, prevention consists of vaccination as well as limiting exposure to wildlife. Please visit your local veterinarian if your pet is not up to date on the rabies vaccine.
Vaccines in Dogs: Distemper (DAPP)
The second core vaccine in dogs is the distemper vaccine (DAPP). This vaccine protects against the Distemper Virus, Parvovirus, Adenovirus 1 & 2, and Parainfluenza virus. The DAPP vaccine is started at 8 weeks of age and must be boostered at least 3 times, 3 to 4 weeks apart.
This means that your puppy will get a DAPP vaccine at 8 weeks,12 weeks, and 16 weeks old. After the initial puppy series, the vaccine becomes annual. It is also available in a 3-year version, which can be the year after your puppy’s initial vaccine series.
Parvovirus is a common viruses affecting puppies. Any puppy with clinical signs consisting of vomiting and diarrhea should be tested for parvovirus. A diagnosis can be made from a fecal sample.
Intensive supportive care is needed to treat a dog that has been infected with parvovirus. Supportive care consists of hospitalization, fluid therapy, antibiotics, anti-nausea medication, anti-diarrheal medication, and monitoring blood work changes (particularly your dog’s white blood cells). Be prepared for a 5- to 7-day hospitalization as well as an expensive bill, depending on the severity of your dog’s illness.
Without treatment, this virus can be fatal. Prevention is cheaper than treatment.
Vaccines in Dogs: Leptospirosis
Although the canine Leptospirosis vaccine is not a core vaccine, it is highly recommended in areas that have a high rodent population. It can be given as early as 12 weeks of age and needs to be boostered 3 to 4 weeks after an initial dose is given. After that, it is given annually.
Dogs can become infected with this bacterium via open wounds or mucus membranes coming into contact with infected urine or infected water or soil. This bacterium can survive for weeks to months in the environment, so it is important to have your pet vaccinated if you live in an area that has a high rodent population.
Leptospirosis is zoonotic, which means that humans can get infected as well. An infection can quickly lead to organ damage and can affect the kidneys and liver. Clinical signs can be very nonspecific, and treatment consists of antibiotics and supportive care. In severe cases infection can lead to irreversible organ damage.
Vaccines in Dogs: Bordetella
The canine Bordetella vaccine covers Canine Kennel Cough. It requires no booster and is given annually, although in some cases it is recommended to be given every 6 months. It can be delivered either intranasally or subcutaneously.
Bordetella is essentially an infectious bronchitis and is spread within respiratory secretions from an infected dog. In crowded situations with many animals, for example, at a boarding or grooming facility, dogs can be more predisposed to infection due to close contact as well as poor ventilation.
Clinical signs can range from mild to severe symptoms, such as a hacking cough and pneumonia. Treatment consists of antibiotics and quarantine. Keep in mind that many boarding and grooming facilities require this vaccine.
Vaccines in Dogs: Canine Influenza Virus
The canine influenza virus (CIV) vaccine requires one additional booster given 3 to 4 weeks after the initial dose. After that, it is given annually. It can be started as early as 16 weeks old.
Clinical signs can be very similar to Bordetella and can include cough, sneezing, and nasal discharge. Outbreaks are most commonly associated with kennels where dogs are in close contact. This virus is spread via nasal secretions. It can be hard to distinguish Bordetella from CIV, so treatment consists of controlling secondary signs and treating symptomatically. That means antibiotics and cough suppressants, depending on the severity.
Vaccines in Dogs: Lyme Disease
The canine Lyme vaccine is a lifestyle vaccine for dogs that frequently go to forest preserves or camping. If you live in a highly wooded area, this vaccine is highly recommended due to tick exposure. It can be given any time after 16 weeks of age and requires one additional booster 3 to 4 weeks after the first dose. After that, it is an annual vaccine.
Lyme disease is spread via a bite from infected ticks. Lyme disease can be diagnosed with a SNAP 4DX heartworm test, which entails a blood sample from your dog. Results are obtained in no more than 8 minutes. However, a positive Lyme result does not differentiate exposure to the disease from active infection.
Clinical signs can vary and can be very nonspecific. These can include fever, fatigue, and swollen joints. Treatment consists of antibiotics and managing secondary symptoms. Don’t forget your dog’s monthly flea and tick preventatives, which can greatly reduce the chance of infection with Lyme disease.

Vaccines in Cats: FVRCP
The Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia (FVRCP) vaccine series, also called the cat distemper vaccine, should be started at 6 to 8 weeks of age. This is boostered every 3 to 4 weeks until your kitten is 16 weeks old. This vaccine is also available in a 3-year version that can be given the year after your kitten’s initial vaccine series.
Feline panleukopenia is similar to parvovirus in dogs. It is a very contagious and life-threatening infectious disease that can spread among cat colonies or cats housed with many other cats. An infected cat sheds the virus via secretions, e.g., feces, vomit, urine, saliva, and mucus membranes. Infection occurs when the virus enters through the nose or mouth.
The virus suppresses the immune system and depletes the cat’s white blood cells, leaving the infected individual immunosuppressed and vulnerable to other infectious diseases. Clinical signs can be nonspecific and include fever, vomiting, diarrhea, and lethargy.
Similar to parvovirus in dogs, treatment of a cat infected with panleukopenia consists of hospitalization, aggressive fluids therapy, antinausea and anti diarrheal medications, and supportive care.
Vaccines in Cats: Feline Leukemia Virus
If your cat is an indoor/outdoor cat, the feline leukemia vaccine is highly recommended due to socialization with other cats. This vaccine requires an additional booster 3 to 4 weeks after initial dose.
Feline leukemia virus (FLV) is spread through close social contact with saliva, blood, urine, or feces. There is no effective treatment, so treatment consists of supportive care. Prognosis after infection can be variable.
One Last Reminder
Vaccinating your dogs and cats is very important. If your pet is not up to date on vaccines or their annual wellness exam, please schedule an appointment with their primary care veterinarian to get their vaccines updated.
And remember, prevention is cheaper than treatment.
—Dr. Angelica Calderon

Vacunas en Perros y Gatos
La prevención es más barata que el tratamiento. Una cita que siempre recordaré del Dr. Vinu, una veterinaria con la que trabajé durante mis estudios en la UIC.
Las vacunas son muy críticas en gatos y perros y sus series se inician a una edad muy temprana, incluso algunas vacunas necesitan ser reforzadas para que la mascota alcance la inmunidad adecuada. Hay muchas vacunas diferentes en gatos y perros. Algunas vacunas son vacunas básicas, lo que significa que se recomiendan para todos los pacientes, y otras se consideran vacunas de estilo de vida, lo que significa que depende de lo que haga su mascota. Su perro se aloja con frecuencia en un centro de alojamiento o va frecuentemente a la peluquería, donde puede estar rodeado de muchos otros perros? Su perro va a reservas forestales o a viajes de campamento donde puede estar expuesto a las garrapatas? Su gato es un gato estrictamente de interior o un gato de interior/exterior? Todas esas son excelentes preguntas que generalmente se hacen al comienzo de su examen anual de bienestar. Sí, es posible que le hagamos muchas preguntas durante el examen de bienestar de su mascota, pero estamos reuniendo las piezas del rompecabezas para recomendar el mejor programa de vacunas para su mascota.
Vacuna contra la Rabia en Perros y Gatos
La ley exige que su mascota sea vacunada contra la rabia. Se recomienda que la vacuna contra la rabia canina y felina se administre a los 4 meses de edad, sin embargo, a veces se puede administrar antes en un refugio. La primera vacuna suele ser una vacuna de 1 año, sin embargo, al año siguiente, su mascota puede recibir la vacuna contra la rabia de 1 año o de 3 años.
La rabia se transmite a través de heridas por mordedura, generalmente por la vida silvestre como zorrillos, murciélagos, mapaches y zorros. El virus se adhiere a las células musculares locales y luego penetra en los nervios locales y asciende al cerebro. No existe un tratamiento eficaz y fiable para la rabia y la infección suele provocar la muerte del animal. Una vez que los signos clínicos están presentes, la muerte puede ocurrir dentro de los 10 días. Si su mascota muerde a otro animal o humano y no está al día con la vacuna contra la rabia, dependiendo de su historial de vacunas, es posible que deba ser confinado y observado en un centro veterinario durante 10 días. Si el animal muestra algún síntoma o se sospecha que la mascota pueda tener rabia, se debe enviar su tejido cerebral para la toma de muestras. Esto significa que deben ser sacrificados humanamente para la presentación de tejido. Las regulaciones pueden variar según el estado o el condado, por lo que es importante mantenerse al día con las regulaciones actuales. Puede visitar rabiesaware.org para obtener más información sobre las regulaciones en su área. En última instancia, la prevención consiste en vacunar y limitar la exposición a la vida silvestre. Visite a su veterinario local si su mascota no está al día con la vacuna contra la rabia.
Vacunas en Perros
Distemper (DAPP):
La segunda vacuna básica en perros es la vacuna contra el distemper(DAPP). Esta vacuna protege contra los virus de distemper, el parvovirus, el adenovirus 1 y 2 y el virus de la parainfluenza. La vacuna DAPP se inicia a las 8 semanas de edad y debe reforzarse al menos 3 veces, con 3-4 semanas de diferencia. Esto significa que su cachorro recibirá la vacuna DAPP a las 8, 12 y 16 semanas de edad. Después de la serie inicial de cachorros, se vuelve anual. Esta vacuna también está disponible en un año 3 que se puede administrar el año siguiente después de la serie inicial de vacunas de sus cachorros.
El parvovirus es uno de los virus más comunes que cubre esta vacuna. Cualquier cachorro con signos clínicos que consisten en vómitos y diarrea debe someterse a una prueba de parvovirus y se puede llegar a un diagnóstico con una muestra fecal. Se necesitan cuidados intensivos para tratar a un perro que ha sido infectado con parvovirus y, en última instancia, el tratamiento es de apoyo. La atención de apoyo consiste en hospitalización, terapia de fluidos, antibióticos, medicamentos contra las náuseas, medicamentos contra la diarrea y el control de los cambios en los análisis de sangre (en particular, los glóbulos blancos de su perro). Esté preparado para una hospitalización de 5 a 7 días, así como para una factura costosa, según la gravedad de los síntomas de su perro. Sin tratamiento, este virus puede ser fatal. La prevención es más barata que el tratamiento.
Leptospirosis:
Aunque la vacuna contra la leptospirosis canina no es una vacuna básica, es muy recomendable en áreas que tienen una alta población de roedores. Puede administrarse tan pronto como a las 12 semanas de edad y debe reforzarse 3 o 4 semanas después de administrar la dosis inicial. Después de eso, se da anualmente.
Los perros pueden infectarse con esta bacteria a través de heridas abiertas o membranas mucosas que entran en contacto con orina infectada o agua o tierra infectada. Esta bacteria puede sobrevivir durante semanas o meses en el medio ambiente, por lo que es importante vacunar a su mascota si vive en un área con una gran población de roedores. La leptospirosis es zoonótica, lo que significa que los humanos también pueden infectarse. Esto puede conducir rápidamente a daños en los órganos y puede afectar los riñones y el hígado. Los signos clínicos pueden ser muy inespecíficos y el tratamiento consiste en antibióticos y atención de apoyo; sin embargo, en casos graves, puede provocar daños irreversibles en los órganos.
Bordetella:
La vacuna canina Bordetella cubre la tos canina. No requiere refuerzo y se administra anualmente, sin embargo en algunos casos se recomienda administrar cada 6 meses. Hay dos formas disponibles, por vía intranasal y por vía subcutánea.
Bordetella es esencialmente una bronquitis infecciosa y se transmite dentro de las secreciones respiratorias de un perro infectado. En situaciones de hacinamiento donde hay muchos animales en una instalación, por ejemplo, alojamiento o aseo, los perros pueden estar más predispuestos a la infección debido al contacto cercano y a la mala ventilación. Los signos clínicos pueden variar desde síntomas leves a graves, como tos seca, hasta neumonía. El tratamiento consiste en antibióticos y cuarentena durante el tratamiento. Tenga en cuenta que muchas instalaciones de alojamiento y aseo requiere esta vacuna.
Virus de la influenza canina (CIV):
La vacuna contra el virus de la influenza canina requiere un refuerzo adicional administrado de 3 a 4 semanas después de la primera dosis inicial, luego de lo cual se vuelve anual. Se puede iniciar desde las 16 semanas de edad.
Los signos clínicos pueden ser muy similares a los de Bordetella y pueden incluir tos, estornudos y secreción nasal. Los brotes se asocian más comúnmente con perreras donde los perros están en contacto cercano con otros perros y este virus se transmite a través de las secreciones nasales. Puede ser difícil distinguir Bordetella de CIV, por lo que el tratamiento consiste en controlar los signos secundarios y tratar sintomáticamente. Eso significa antibióticos y supresores de la tos, según la gravedad.
Lyme:
La vacuna canina de Lyme es una vacuna de estilo de vida. Esto significa que si tu perro va con frecuencia a reservas forestales o a acampar, o si vives en una zona muy boscosa, es muy recomendable debido a la exposición a las garrapatas. Se puede administrar en cualquier momento después de las 16 semanas de edad y requiere un refuerzo adicional de 3 a 4 semanas después de la primera dosis inicial. Después de eso, es una vacuna anual.
La enfermedad de Lyme se transmite a través de una picadura de garrapatas infectadas. La enfermedad de Lyme se puede diagnosticar con una prueba de gusano del corazón SNAP 4DX, que implica una muestra de sangre para su perro. Los resultados se obtienen en no más de 7-8 minutos. Sin embargo, incluso si su perro tiene un resultado positivo de Lyme, eso no diferencia la exposición frente a la infección activa. Los signos clínicos pueden variar y pueden ser muy inespecíficos. Estos pueden incluir fiebre, fatiga, articulaciones inflamadas, etc. El tratamiento consiste en antibióticos y el control de los síntomas secundarios. No olvide los preventivos mensuales contra pulgas y garrapatas de sus perros, ya que pueden reducir en gran medida la posibilidad de infección con la enfermedad de Lyme.

Vacunas en Gatos
FVRCP:
La serie de vacunas FVRCP (moquillo felino) debe comenzar a las 6-8 semanas de edad. Esta vacuna requiere refuerzos y se refuerza cada 3-4 semanas hasta que tu gatito tenga 16 semanas. Esta vacuna también está disponible en un año 3 que se puede administrar el año siguiente después de la serie inicial de vacunas de sus gatitos.
FVRCP significa rinotraqueítis viral felina, calicivirus y panleucopenia. La panleucopenia felina es similar al parvovirus en perros. Esta es una enfermedad infecciosa muy contagiosa y potencialmente mortal que puede afectar a las colonias de gatos o a los gatos alojados con muchos otros gatos si una persona está infectada. Un gato infectado elimina el virus a través de secreciones, que incluyen heces, vómito, orina, saliva y membranas mucosas. La infección se produce cuando el virus entra por la nariz o la boca. El virus suprime el sistema inmunológico y agota los glóbulos blancos del gato, dejando al individuo infectado inmunosuprimido y vulnerable a otras enfermedades infecciosas. Los signos clínicos pueden ser inespecíficos e incluyen fiebre, vómitos, diarrea y letargo. Similar al parvovirus en perros, el tratamiento de un gato infectado con panleucopenia consiste en hospitalización, fluidoterapia agresiva, así como antináuseas, antidiarreicas y atención de apoyo.
Virus de la leucemia felina
Si su gato es un gato de interior/exterior, la vacuna contra la leucemia felina es muy recomendable debido a la socialización con otros gatos. Esta vacuna requiere un refuerzo adicional de 3 a 4 semanas después de la dosis inicial.
FeLV (virus de la leucemia felina) se propaga a través del contacto social cercano con saliva, sangre, orina, heces. No existe un tratamiento eficaz, por lo que el tratamiento consiste en cuidados de apoyo. El pronóstico después de la infección puede ser variable.
Es muy importante vacunar a sus perros y gatos. Si su mascota no está al día con las vacunas o su examen anual de bienestar, programe una cita con su veterinario de atención primaria para actualizar sus vacunas.
Y recuerda, la prevención es más barata que el tratamiento.
—Dr. Angelica Calderon
Hyperthyroidism in Cats: Is This Why Your Older Cat Is Skinny?
Hyperthyroidism is the most common endocrine disease in middle-aged and senior cats. It is typically diagnosed when the cat is 12 to 13 years old.
Like the name implies, hyperthyroidism is the increased production and secretion of thyroid hormones from an abnormally functioning and enlarged thyroid gland. Because thyroid hormones affect almost every organ in a cat’s body, having excessive hormones typically causes secondary health issues, such as heart disease and high blood pressure. Hyperthyroidism can also mask kidney disease in cats.
In most cases, this disease is caused by a non-cancerous tumor, called an adenoma, on the thyroid gland. The exact cause of this disease in cats is not currently known.
Clinical Signs and Diagnosis
The most common sign of hyperthyroidism is weight loss in the face of an increased appetite. Over time, a cat with hyperthyroidism will become increasingly skinnier and may also lose muscle mass.
These cats may also experience increased thirst and urination, changes to their hair coat quality (more greasy, matted, or unkempt), vomiting, diarrhea, and increased vocalization.
Diagnosis of hyperthyroidism is through a complete physical examination as well as lab testing (complete blood count, chemistry, urinalysis, and thyroid hormones). If cat has hyperthyroidism, a thyroid hormone called T4 will be elevated on these lab tests.
Treatment
There are currently four methods of treatment for hyperthyroidism; all have the goal of returning thyroid hormone levels to normal. Treatment options include medical therapy with antithyroid drugs; dietary therapy with iodine-restricted diets; surgical removal of the thyroid gland; and radioactive iodine therapy.
Medical Therapy
Methimazole is the most common anti-thyroid medication. It reduces the production and release of thyroid hormone from the thyroid gland. This therapy does not serve as a cure for the disease but allows for control.
Methimazole is relatively inexpensive and is either administered orally or as a transdermal gel that is applied to the ear. Both forms of medication are given twice a day. Some cats experience side effects of this medication within the first few months of starting it. These include vomiting, decreased appetite, lethargy, and skin itchiness that causes the cat to scratch and wound their face.
While on methimazole, repeated blood monitoring must be done to ensure the proper dosage is being used as well as to monitor kidney function and overall health. During the first 2 to 3 months of treatment, lab testing is done every 2 to 3 weeks. After thyroid hormone levels have normalized, monitoring is then done every 3 to 6 months.
Dietary Therapy
Feeding an iodine-restricted diet is another therapeutic option. This approach works because iodine is needed for the body to produce thyroid hormones. For the best results, this diet must be fed exclusively and consistently. These diets have been shown to reduce the levels of thyroid hormones in 3 to 4 weeks. If normal thyroid hormone levels are not achieved within 12 weeks, a different form of treatment is usually selected. Dietary therapy is not effective if the cat does not like to eat the food or regularly has access to other forms of food.
Surgery
Removal of the thyroid glands is another form of treatment. It is a straightforward procedure for a skilled surgeon and has a good success rate. Surgery has the advantage of being curative and eliminating the need for long-term medication administration. A risk of surgery is accidental damage to the parathyroid glands, which are located close to the thyroid glands. If the parathyroid glands are damaged, the cat’s body will have difficulty producing calcium. Because less invasive treatment options are available, surgery is rarely selected for treatment.
Radioactive Iodine Therapy
Radioactive iodine therapy is currently considered the treatment of choice for cats with hyperthyroidism. Radioactive iodine is given as an injection, which then travels through the bloodstream to the thyroid gland. The radiation from the radioactive iodine then destroys the abnormal thyroid tissue without damaging the surrounding healthy tissue.
The radioactivity does not harm the cat but does pose a risk for humans. Due to this, cats undergoing this treatment are hospitalized for 3 to 5 days after treatment until the radiation levels are low. Cats are not allowed visitors during this time. In 95% of cases, this treatment is curative within 3 months. If not successful, the treatment can be repeated. In rare cases, a cat can become hypothyroid (producing too low levels of thyroid hormone), which then must be treated with thyroid hormone supplement.
Prognosis
Once hyperthyroidism is diagnosed and a form of treatment is selected, most cats do well. As medical therapy and dietary therapy are not curative, treatment is lifelong in these cases. Surgery and radioactive iodine therapy are considered curative, so lifelong treatment is not needed.
If your cat is experiencing any of the clinical signs mentioned, please reach out to your veterinarian to have your cat tested. If your cat is diagnosed with hyperthyroidism, you and your veterinarian can determine the best treatment option for your cat.
—Jeanette Barragan, DVM
Featured photo by Ekaterina Zagorska on Unsplash
Heartworms/Parásitos del Corazón

En español
Con el verano acercándose, muchos de nosotros pensamos en el riesgo de las pulgas, garrapatas y parásitos intestinales pero no se olviden de los parásitos del corazón! El parásito del corazón es transmitido por los mosquitos y causa daño irreversible al corazón, las arterias, y los pulmones. No existe cura en los gatos y el tratamiento en los perros es costoso, doloroso, y toma un promedio de un año.
Muchos piensan que sus mascotas no están a riesgo de infección en Illinois como tenemos inviernos largos, pero solo se necesita una mordida de un mosquito que lleva el parásito para ser infectado. Aunque su mascota no salga de la casa, los mosquitos pueden entrar por las ventanas, garajes, puertas, etc.
Es importante realizar que la prevención no previene la exposición y aunque los medicamentos preventivos no matan al parásito adulto, se usan para prevenir la madurez de los gusanos. Si el medicamento preventivo se da sin prueba de diagnóstico y el perro está infectado, no solo se quedará infectado pero también puede causar reacción parecida a un shock. En casos inusuales, también puede resultar en fallecimiento de la mascota.
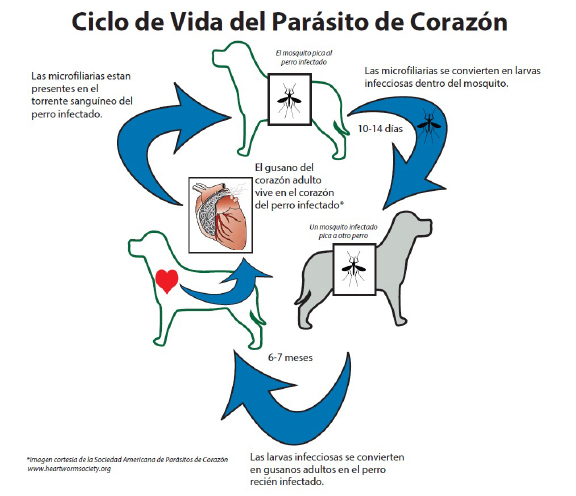
Los gusanos adultos parecen espagueti cocido y pueden llegar a 12 pulgadas. La carga parasitaria puede variar de 1 a 250 gusanos con un promedio en los perros de 15 gusanos! La severidad de los síntomas depende de la carga parasitaria, el nivel de actividad de la mascota, y cuánto tiempo ha estado infectado. Los síntomas más comunes son tos, dificultad para respirar, fatiga, falta de apetito, y pérdida de peso.
El mejor tratamiento es la prevención!
La buena noticia es que existen varios medicamentos preventivos para los perros y gatos! Se necesita una prueba negativa una vez al año (en los perros) para poder recetar el medicamento. Si su mascota no ha tomado la prevención del parásito del corazón de manera constante durante los últimos 12 meses, debería hacer una cita con su veterinario para hacer un análisis de sangre para comprobar un resultado negativo y poder recetar prevención. Hay varias formas de prevención y su veterinario le puede recomendar cual usar basada en su estilo de vida.
In English
With summer approaching, many of us think about the risk of fleas, ticks, and intestinal worms. But don’t forget about heartworms! Heartworms are transmitted by mosquitoes and cause irreversible damage to the heart, arteries, and lungs. There is no cure in cats, and treatment in dogs is expensive, painful, and takes an average of one year.
Many think that their pets are not at risk of infection in Illinois since we have long winters, but it only takes one bite from a mosquito that carries the parasite to be infected. Even if your pet does not leave the house, mosquitoes can enter through windows, garages, doors, etc.
It is important to realize that prevention does not prevent exposure. Although preventative medications do not kill the adult parasite, they are used to prevent the worms from maturing. If the preventative medication is given without a diagnostic test when the dog is already infected, the dog will not only stay infected but the medication can also lead to a shock-like reaction. In rare cases, it can also result in the death of the pet.
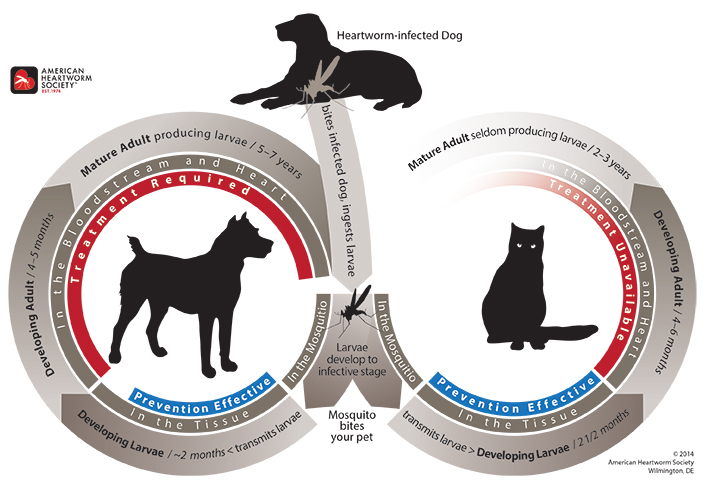
Adult worms look like cooked spaghetti and can grow to 12 inches. The parasite load can range from 1 to 250 worms, with an average of 15 worms in dogs! The severity of the symptoms depends on the parasitic load, the pet’s activity level, and how long they have been infected. The most common symptoms of a heartworm infection are cough, shortness of breath, fatigue, lack of appetite, and weight loss.
The best treatment is prevention!
The good news is that there are several preventative medications for dogs and cats! A negative test is needed once a year (in dogs) before the drug can be prescribed. If your pet has not been on heartworm prevention consistently for the past 12 months, you should make an appointment with your veterinarian for a blood test to confirm a negative result so prevention can be prescribed. There are various forms of prevention, and your vet can recommend which one to use based on your lifestyle.
– Dr. Ana Valbuena
Even Vets Sometimes Need Vets

I need to come clean: I’m a bit of a lazy dog owner. I don’t brush Emmie’s teeth, I’m usually a few days late to remember her heartworm, flea, and tick preventatives, and we only did the bare minimum with training to curb Emmie’s issue with meeting strangers.
COVID Shut Down Puppy Socialization
Like most of you, our lives drastically changed March 2020. Not only did COVID become part of our lives, but we also welcomed our first daughter. (My first time leaving the house without her to run an errand was the day the governor shut the state down.)
So, what little progress we made with Emmie meeting strangers and with getting her used to people coming into the house went out the window. And my family wasn’t not alone.
Now that many people are heading back to work, we are seeing a lot more behavioral issues with pets as they are trying to adjust to post COVID life. For my family, this transition has been tough, because now not only do we have a dog that is even worse with strangers, but we must think about playdates with handsy toddlers with underdeveloped pre-frontal cortexes.
Time to Ask for Help
We were at a loss. The thought even crossed my mind that we may need to rehome our dog. I’ve helped a lot of clients manage routine behavioral issues, but some issues require looking to veterinarians who have more training and certification in their specialties.

So that’s what my family did. We have started working with a boarded veterinary behaviorist. You may have found being referred to a specialist frustrating (and at times expensive) when I or one of my colleagues recommended that. However, please know that it’s because we want what’s best for your pet. And sometimes, we don’t have that particular skill set. Even we need help sometimes.
We have a long road ahead of us with Emmie, but I’m hoping that as we welcome our second daughter to our family this summer, with some training and tweaking medications, things will get better. I’m hoping that maybe this time around, my maternity leave will involve having more family and friends meet our baby girl in person instead of over Zoom.
Bringing Home (Another) Baby
This is probably a good time to mention that I will be on leave from the end of June (unless this little one decides to come early) through the end of October. I would also like to thank our medical director, Dr. Sullivan, for being so supportive with scheduling my leave and return to work. And the amazing staff at Medical District Veterinary Clinic have been so supportive and helpful as they watch me waddle from patient to patient, never complaining that I’m not as able to help with certain tasks, which means more work for them.
I am so grateful to be part of this incredible team, and although I am looking forward to having a warm summer, pandemic-free (fingers crossed) maternity leave, I know I will be excited to come back in the fall.
— Dr. Alyssa Kritzman
The State of the Medical District Veterinary Clinic
(from Dr. Sullivan’s perspective)

We’ve Seen Some Changes
Change was happening within the veterinary profession even before the pandemic, but change has drastically accelerated over the past four years.
Today, there is a veterinarian and veterinary staff shortage, expenses have increased more than inflation, and the demand for veterinary care has increased. This has resulted in overworked and tired veterinary professionals.
At Medical District Veterinary Clinic, we have always striven to maintain a healthy work-life balance for our staff. Despite these recent challenges, we remain committed to that goal. This blog post shares the facts about the impact of changes on our clinic and what that means for our clients.
Lots of Growth in Veterinary Medicine
Since the start of the pandemic there has been:
- An increase in demand for veterinary services (and an increase in consumer spending overall)
- An increase in pet ownership in the US, from 67% of households to 70% of households (according to US News and World Report)
- An increase in spending on pets in the US, jumping 19% between 2020 and 2021 for a total of $123.6 billion annually (according to Forbes)
On grooming, pet food, veterinary care, and luxury pet items, households are spending more than ever before. The largest group of pet owners is millennials, making up 32% of pet owners, followed by baby boomers at 27%.
While on the surface, this sounds great for the veterinary industry, it has resulted in stress across the profession. Veterinarians, veterinary technicians, and support staff have been stretched thin. The staffing issues that already existed within the profession were made worse by the acute, dramatic change in demand.
Growth at Medical District Vet Clinic
Things were no different at our practice. At the height of the staffing challenges, we had veterinarians and support staff seek positions at other practices, leaving us short-staffed and unable to meet our client demand. Unfortunately, this resulted in our inability to meet all our patients’ needs, and we had to deal with many frustrated and upset clients. As a result, staff and veterinarians were further discouraged and facing burnout.
Fortunately, we were able to recruit and hire three veterinarians and three certified veterinary technicians. We are very lucky to be in a position to offer competitive salary and benefits packages to aid in recruitment. We are now fully staffed and able to provide staff with work-life balance while also having availability to see patients in a timely manner.
But Also Some Negative Developments
Negative effects on the veterinary industry since COVID include large increases in both overall expenses and no-show appointments.
A trend for increased veterinary expenses over the past few years saw the biggest bump up in late 2022/early 2023. Drug and medical supplies, laboratory costs, and staffing costs have all increased. Total costs have increased at a rate higher than US inflation.

We have also seen a disappointing client trend, at our clinic and across the industry: a large increase in no-show appointments. We noticed this trend months ago and started tracking no-shows. We changed our confirmation protocol to help owners remember upcoming appointments, but that did not seem to make much difference.
March 2023 was by far our worst month: we had 92 no-shows. This is 92 more patients we could have helped or not had to refer to an emergency clinic if clients would have just called to let us know they would not be coming. As an existing client, you might be thinking this issue must be related to new clients, and you are partially correct. However, almost two-thirds of our no-shows are existing clients.
To combat this alarming new trend, we and other practices have implemented measures including cancellation/no-show fees or deposits required to book appointments.
How We Are Responding to These Trends
So what changes you can expect at the Medical District Veterinary Clinic? We will continue to strive to provide exceptional, high-quality veterinary care, while also providing our staff with the support to maintain a healthy work-life balance.
Because of the overall increase in expenses, we must increase prices to meet our costs. However, our prices for long-term medications will continue to match PetMeds’ online prices (see chart). Offering these medications at competitive prices provides convenience to our clients and allows us to help with clients’ issues or questions regarding pharmaceuticals. You also help us maintain that revenue stream when you purchase your pet’s medications from us instead of online.
| PetMeds Price-Matched Medications |
|---|
| Heartgard Plus (6/12 packs) |
| Sentinel Spectrum (6/12 packs) |
| NexGard (6/12 packs) |
| Simparica Trio (6/12 packs) |
| Senergy Cats (6/12 packs) |
| Rimadyl Chewable Tablets (60/90/180 count) |
| Deramaxx Chewable tablets (30/60/90 count) |
Beginning in May, we will also be instituting a deposit to book an appointment for all new clients as well as for existing clients who have a history of no-show.
We understand that sometimes life gets in the way, things happen, and clients may occasionally miss appointments. Unfortunately, the trends we are seeing have left us without another option. The deposit will be refundable if the appointment is canceled prior to 24 hours before the scheduled appointment. Please see here for the complete policy.
Thank you!
Lastly, I want to thank you all for trusting us in caring for your pets. I can speak on behalf of all the staff at Medical District Veterinary Clinic: We truly love what we do and daily have your pet’s best interest in mind.
Please don’t hesitate to reach out with any questions or concerns. Or compliments! Compliments for staff and doctors are always greatly appreciated.
Truly,
Drew Sullivan, DVM
Director, Medical District Veterinary Clinic
The Itchy Pet
Para leer el blog en español, haga clic aquí

With Chicago’s changing weather, who knows what season we’re currently in right now? And with the season change comes … seasonal allergies, or just allergies in general.
That’s the tricky part that we veterinarians face. We have to investigate and determine what type of allergies your pet is experiencing, and if it is truly allergies versus something else.
As many of you may know, just like people get allergies, so do pets. The signs, however, can be a little different. Many times your pet will show signs of scratching, biting, chewing, and rubbing certain areas of their bodies. You can even see redness, inflammation, fur loss, and, in severe cases, open, infected wounds.
There are many components to allergies, and getting a detailed history from you during the initial vet visit is very important. So although it may seem like an interrogation in the exam room, this is when we are putting all of the puzzle pieces together in our head and thinking of the best diagnostic tests and treatment options for your pet. Each pet is different, and treatment varies on a case-by-case basis.
Flea Allergy
“My cat doesn’t go outside.” “My dog isn’t around other dogs.” “I’ve never seen any fleas on my pet.”

Just because you don’t see them, doesn’t mean they’re not there. Did you know that 1 female flea can lay between 20 and 50 eggs a day?
At times, the only evidence we have to suspect that there are fleas present is flea dirt, which is basically flea feces. Areas that can be affected by fleas include the tail base, neck region, and belly, although fleas can be found anywhere on the body.
A flea allergy is caused by the saliva of the flea itself. All it takes is a few bites to see clinical signs. Fleas can survive at a wide range of temperatures, so it is important to have your pet on flea and tick preventatives year-round to avoid flea allergy dermatitis. Read more about fleas.
Food Allergy
Pets can also have hypersensitivities to certain foods. Although potential allergens can include the food dye, carbohydrates, or preservatives, often it’s the protein source that is the culprit. A food allergy is diagnosed based on a detailed history and, most importantly, a strict food trial.

A food trial consists of feeding your pet a hydrolyzed diet or novel protein for a minimum of 8 weeks. This diet is very strict, and it is important that you only feed the novel protein or hydrolyzed diet. You must not feed any additional foods or treats. Keep in mind that many medications and monthly preventatives can be flavored so you must monitor closely what you are feeding and giving your pet. If after the trial period your pet is symptom free, a food challenge is performed. This consists of introducing the previously fed diet and watching for signs of itching or scratching. More details regarding a food trial can be discussed with your veterinarian. Read more about food allergies.
Seasonal vs Environmental Allergies
These can get tricky and hard to diagnose so, as previously mentioned, a thorough history becomes very important. We must investigate if there is any pattern to the clinical signs. Are the signs happening when it is warmer out vs colder? Do the signs show up after walks or after visiting certain areas, like a park or forest preserve? Every detail matters, so it is important to reach out to your veterinarian when your pet starts experiencing signs of excessive itching, scratching, licking, fur thinning, etc.
Treatment for Allergies
Treatment varies on a case-by-case basis. Ultimately, we want to control your pet’s clinical signs but also make your pet comfortable and clear of any secondary infections. Contact your local veterinarian when you start seeing any of the previously mentioned clinical signs.
There are several allergy medications to try. Each pet is different, and sometimes it can take some trial and error to find what works best for your pet, whether that is a single medication or a combination of medications. Allergy medications come in oral, injectable, and topical formats. Your veterinarian will determine which one suits you and your pet’s lifestyle.
Is It Even Allergies?
Although fur loss, fur thinning, over-grooming, and biting can be signs of allergies, these can also be signs of stress, especially in cats. Fur thinning and fur loss can even be signs of endocrine diseases, such as hyperthyroidism or hypothyroidism.
If your pet is experiencing any of the clinical signs mentioned throughout this post, please reach out to your veterinarian so they can determine the best diagnostic test and treatment options for your pet. You and your veterinarian form a team that wants the best for your pet.
– Dr. Angelica Calderon
Comezón de la mascota
Con el clima cambiante de Chicago, quién sabe en qué temporada estamos ahora. Y con el cambio de clima llegan… las alergias. Esa es la parte difícil a la que nos enfrentamos los veterinarios. Tenemos que investigar y determinar qué tipo de alergias está teniendo su mascota y si realmente se trata de alergias o de otra cosa.
Como muchos de ustedes saben, al igual que nosotros podemos tener alergias, las mascotas también pueden hacerlo. Sin embargo, nuestros signos pueden ser un poco diferentes. Muchas veces su mascota puede mostrar signos de rascarse, morderse, y masticar ciertas áreas de su cuerpo. Incluso se puede ver enrojecimiento, inflamación, pérdida de pelo y, en casos graves, heridas abiertas infectadas.
Las alergias tienen muchos componentes y es muy importante obtener un historial detallado durante la visita inicial al veterinario. Entonces, aunque pueda parecer un interrogatorio en la sala de examen, al mismo tiempo estamos juntando todas las piezas del rompecabezas en nuestra cabeza y pensando en las mejores pruebas de diagnóstico y opciones de tratamiento para su mascota, ya que cada mascota es diferente y puede variar según el caso.
Alergia a las pulgas

“Mi gato no sale”, “Mi perro no está con otros perros”, “Nunca he visto pulgas en mi mascota”. Que no los veas no significa que no estén ahí. ¿Sabías que una pulga hembra puede poner aproximadamente de 20 a 50 huevos por día? A veces, la única evidencia que tenemos para sospechar que hay pulgas presentes es la suciedad de pulgas, que es básicamente heces de pulgas. Las áreas que pueden verse afectadas por las pulgas incluyen la base de la cola, la región del cuello y el vientre; aunque se pueden encontrar en cualquier parte del cuerpo. Una alergia a las pulgas es causada por la saliva de la pulga y nada más se necesita algunas picaduras para ver los signos clínicos. Las pulgas pueden sobrevivir en un amplio rango de temperaturas, por lo que es importante que su mascota tome medicamentos preventivos contra pulgas y garrapatas durante todo el año para evitar la dermatitis alérgica por pulgas. Leer más sobre pulgas.
Alergia a la comida

Las mascotas también pueden tener hipersensibilidad a ciertos alimentos. Aunque los alérgenos potenciales pueden incluir colorantes alimentarios, carbohidratos o conservantes; lo más común es la proteína que es la culpable. Una alergia alimentaria se diagnostica en base a un historial detallado y una prueba alimentaria estricta. Una prueba de alimentación consiste en alimentar a tu mascota con una dieta hidrolizada o proteína novedosa durante un mínimo de 8 semanas. Esta dieta es muy estricta y es importante que solo le des la dieta proteica o hidrolizada novedosa. No debe alimentar con alimentos adicionales. Tenga en cuenta que muchos medicamentos y preventivos mensuales pueden tener sabor, por lo que debe controlar de cerca lo que alimenta y le da a su mascota. Si tu mascota está asintomática, se realiza un reto alimentario que consiste en introducir la dieta alimentada previamente y vigilar si presenta signos de picor o rascado. Se pueden discutir más detalles sobre una prueba de alimentos con su veterinario. Leer más sobre alergias alimentarias.
Alergias Estacionales y Ambientales
Estos pueden volverse complicados y difíciles de diagnosticar, por lo que como se mencionó anteriormente, un historial completo y detallado se vuelve muy importante. Debemos investigar si existe algún patrón en los signos clínicos. ¿Están ocurriendo los signos cuando hace más calor que cuando hace más frío? ¿Aparecen los signos después de caminatas o después de visitar ciertas áreas como un parque o una reserva forestal? Cada detalle es importante por lo que es importante comunicarse con su veterinario cuando su mascota comience a enseñar signos de picazón excesiva, rascado, lamido, adelgazamiento del pelaje, etc.
Tratamiento para Alergias
El tratamiento varía según el caso. Queremos controlar los signos clínicos de sus mascotas, pero también hacer que su mascota se sienta cómoda y libre de infecciones secundarias. Esto significa comunicarse con su veterinario local cuando comience a ver cualquiera de los signos clínicos mencionados anteriormente. Hay varios medicamentos para la alergia para probar, sin embargo, cada mascota es diferente y, a veces, puede tomar un poco de prueba y error para finalmente encontrar lo que funciona mejor para su mascota. Qué puede significar un solo medicamento o una combinación de diferentes medicamentos. En cuanto a los medicamentos, hay varias opciones orales para probar, así como opciones inyectables y opciones tópicas. Su veterinario determinará cuál se adapta mejor a usted y al estilo de vida de su mascota.
¿Es incluso alergias?
Aunque la pérdida de pelaje, el adelgazamiento del pelaje, el aseo excesivo y las mordeduras pueden ser signos de alergias; estos también pueden ser signos de estrés, principalmente en gatos. El adelgazamiento y la pérdida de pelo pueden incluso ser signos de varias enfermedades endocrinas como el hipertiroidismo o el hipotiroidismo.
Si su mascota enseña alguno de los signos clínicos mencionados en esta publicación, comuníquese con su veterinario para que pueda determinar las mejores opciones de prueba de diagnóstico y tratamiento para su mascota. Somos un equipo y queremos lo mejor para tu mascota.
– Dr. Angelica Calderon
Osteoarthritis: It’s Not Just for Older Pets

Osteoarthritis in pets is often thought of as a geriatric pet disease that warrants treatment when our pets are obviously painful and experiencing lameness. However, osteoarthritis often starts younger than you might expect, and pain may be present even before lameness is apparent.
Let’s start with what osteoarthritis is: it’s the most common form of arthritis and it is characterized by painful inflammation and degeneration of one or more joints. Over time, it can lead to bone-on-bone contact.
Many factors contribute to the disease process, including overweight or obesity, abnormal joint development, past injury or orthopedic surgery, and how a pet is built.
In dogs, early signs of this disease can include:
- restlessness or irritability,
- frequent position changes during rest,
- not as fast getting up or sitting down,
- weight shifting while standing,
- less interest in activity or play, and
- hesitation before walking, sitting, or climbing stairs.
Eventually, a dog may begin to limp, to experience stiffness when walking, and to have difficulty going up or down stairs and jumping up or down.
In cats, osteoarthritis may look like a reduction in play, grooming, socializing, and appetite, with increases in hiding and sleeping and changes in urination/defecation habits. Cats can also have trouble jumping up/down, climbing up or down stairs, running, and chasing objects.
Because this disease is painful and progressive, early diagnosis and treatment are important for long-term pain management and slowing the progression of the disease. Treatment includes a combination of pain medication, weight loss or maintenance, dietary changes, environmental modification, and exercise.
If you feel your pet may be showing signs of osteoarthritis, our clinic can share additional resources on how to know if your pet has this disease and talk with you about treatment options.
– Dr. Jeanette Barragan
Photo by Madalyn Cox on Unsplash
Keeping Pets Safe for the Holidays

Lee esto en español —>
Happy Paw-lidays! As festivities begin, we want all involved to have a joyful and safe holiday season. Here are some tips to help you keep your four-legged loved ones out of mischief:
No Pawcuterie Boards, Please!
Many already know chocolate is a big no-no for our pets, but keep in mind that almost all human food is high in fat content—and that can lead to big issues! Keep any alcohol, bones, fatty, sweet, or spicy foods in places your pet cannot reach. Visit the ASPCA website for some great information on what not to feed
Instead of human food, consider keeping the dinner portion of your pet’s food in a container for yourself and your guests to use as “treats” throughout the evening.
Instead of showing your love through food, consider switching out toys (perfect excuse for an early gift), adding catnip to some new or old favorite ones, or looking up some fun DIY food puzzles to make with the family!
Tempting Trash
Keep trash away from your pets by securing the lids or taking it out immediately. Think about what we’re likely to throw away…
- Fats and bones can lead to obstructions, pancreatitis, vomiting, diarrhea, and other issues that can result in a veterinary emergency.
- Leftover dough can rise in your pet’s belly and cause bloat.
- Leftover sweets can contain xylitol (sugar substitute), which can cause low blood sugar, seizures, liver failure, or even death.
- Strings/tinsel, aluminum foil, plastic wraps, and broken ornaments/glass can cause foreign body obstructions and serious injuries.
- Old batteries can cause acid burns all the way from the mouth to the stomach!
Open Flames and Toxic Essential Oils
Keep your eye on any open flames, including menorahs, scented candles, stoves, or fireplaces, and keep them out of reach, since you are more likely to be distracted during this busy time.
Essential oils are not only irritating to our pets’ sensitive noses, but cats can absorb the oils through their skin or lick it off their fur after it has been diffused in the air. Toxicity can occur quickly or after prolonged exposure.
- Cinnamon, citrus, peppermint, pine, pennyroyal, sweet birch, tea tree (malaleuca), wintergreen, and ylang ylang oils are all toxic to cats.
Instead of essential oils to scent your home, consider baking cookies right before guests arrive (or every night; we don’t judge).
Holiday Paw-ties and Decor
- Christmas trees
- Keep secure by tying to the ceiling or doorframe and secure with a sturdy tree stand. Cat parent pro tip: Place horizontal and vertical scratching posts near the tree. Providing both types of scratching posts will increase the chances of your kitty using the post instead of the tree!Do not allow your pets to drink the water from live trees as this can cause gastrointestinal upset. Also, do not add aspirin, sugar, or any other additives to the water.
- Keep tinsel and ornaments that can be broken or that are made from food-based materials (such as salt-dough) out of reach of pets to avoid injuries such as intestinal blockage.
- Electrical cords and lights
- Chewing on the cords and lights can cause severe burns. Consider covering the cords with PVC pipes, offering alternatives like chew toys and treats, or using pet-safe bitter spray to keep from chewing cords.
- Unplug decorations when not in use.
- Flowers and festive plants
- Many common holiday plants can be poisonous to pets if ingested. Visit the ASPCA Animal Poison Control Center for a list of plants that are toxic to dogs and cats.
This time of year can also be louder than usual at home and in the neighborhood. For information on helping your pets get through loud noises, such as fireworks, see our June blog post.
We will be closed from December 24 through 27 and from December 31 through January 2, so please contact your local 24/7 clinic or call ASPCA or the Pet Poison Helpline (see numbers below) if you’re unsure of next steps. While consultation fees may apply (usually between $65 and $75), knowing the next steps for the health of your pet is priceless!
ASPCA Poison Control: (888) 426-4435
365 days a year, 24/7
Pet Poison Helpline: (855) 764-7661
365 days a year, 24/7
– Dr. Ana Valbuena
Como mantener las mascotas seguras durante los días festivos!
¡Felices fiestas! ¡A medida que comienzan las festividades, queremos que todos los involucrados tengan una temporada navideña alegre y segura! Aquí hay algunos consejos para ayudarlo a mantener a sus seres queridos de cuatro patas fuera de las travesuras:
¡No a las tablas de ‘pawcuterie’, por favor!
- Muchos ya saben que no se les puede dar chocolate a nuestras mascotas, pero tenga en cuenta que casi todos los alimentos humanos son altos en contenido de grasa y pueden causar problemas. Mantenga cualquier tipo de alcohol, huesos, alimentos grasosos, dulces o comidas picantes en lugares fuera del alcance de sus mascotas. Visite el sitio web de ASPCA para más información sobre alimentos a evitar.
- En lugar de comida humana, considere mantener la porción de la cena de sus mascotas en un recipiente para usarlo como “golosinas” durante toda la noche.
- En lugar de mostrar su amor a través de la comida, considere cambiar los juguetes (excusa perfecta para un regalo temprano), agregar ‘catnip’, o comprar/’DIY’/hacer rompecabezas de comida con la familia.
Basura tentadora
- Mantenga la basura alejada de sus mascotas asegurando las tapas o sacándola inmediatamente. Piensa en lo que es probable que tiremos a la basura…
- Grasas y huesos pueden provocar obstrucciones, pancreatitis, vómitos, diarrea y otros problemas que pueden resultar en una emergencia veterinaria.
- La masa sobrante puede elevarse en el vientre de sus mascotas y causar distensión abdominal.
- Los dulces pueden contener xilitol (sustituto del azúcar), que puede causar niveles bajos de azúcar en la sangre, convulsiones, insuficiencia hepática o incluso la muerte.
- Las cuerdas / oropel, el papel de aluminio, las envolturas de plástico y los adornos / vidrios rotos pueden causar obstrucciones y lesiones graves.
- Las baterías viejas pueden causar quemaduras de ácido desde la boca hasta el estómago.
Llamas abiertas y aceites esenciales tóxicos
- Mantenga su ojo en cualquier llama abierta como menorás, velas perfumadas, estufas o chimeneas durante esta temporada y manténgalas fuera de su alcance, ya que es más probable que nos distraigamos durante este tiempo.
- Los aceites esenciales no solo son irritantes para la nariz sensible de nuestras mascotas, sino que los gatos pueden absorber los aceites a través de su piel o lamerlo de su pelaje después de ser difundidos en el aire: la toxicidad puede ocurrir rápidamente o después de una exposición prolongada.
- La canela, los cítricos, la menta, el pino, el poleo, el abedul dulce, el árbol de té (malaleuca), la gaulteria y los aceites de ylang ylang son tóxicos para los gatos.
- En lugar de aceites esenciales, considere hornear galletas justo antes de que lleguen los invitados (o todas las noches- no juzgamos).
Fiestas y decoración navideña
- Árboles de Navidad
- Asegure el árbol navideño atándolo al techo o al marco de la puerta y asegúrelo con un soporte de árbol resistente.
- Consejo profesional para padres de gato: coloque un poste de rascado horizontal y vertical cerca del árbol
- ¡Proporcionar ambos tipos de postes para rascar aumentará las posibilidades de que su gatito use el poste en lugar del árbol!
- No permita que sus mascotas beban el agua de los árboles vivos, ya que esto puede causar malestar gastrointestinal.
- No agregue aspirina, azúcar o cualquier otro aditivo al agua.
- Mantener los adornos y el oropel que se pueden romper o hacer de materiales a base de alimentos, como la masa de sal, debe mantenerse fuera del alcance de las mascotas para evitar lesiones como la obstrucción intestinal.
- Cables eléctricos y luces
- Masticar los cables y las luces puede causar quemaduras graves, así que considere cubrir los cables con tubos de PVC, ofrezca otras alternativas de masticación como juguetes y golosinas, o compre aerosol amargo que sea seguro para mascotas.
- Desenchufe las decoraciones cuando no estén en uso.
- Flores y plantas festivas
- Muchas plantas navideñas pueden ser venenosas para las mascotas si se ingieren. Visite ASPCA para obtener una lista de plantas que son tóxicas para perros y gatos.
¡Esta época del año también puede ser más ruidosa de lo habitual en casa y en el vecindario! Para obtener más información sobre cómo ayudar a sus mascotas a superar ruidos fuertes como los fuegos artificiales, ¡consulte nuestra publicación de junio!
Estaremos cerrados del 24 al 27 de Diciembre y del 31 de Diciembre al 2 de Enero, así que comuníquese con su clínica local las 24 horas del día, los 7 días de la semana o llame a ASPCA o a la línea de ayuda de envenenamiento para mascotas (consulte los números a continuación) si no está seguro de los próximos pasos. Se pueden aplicar tarifas de consulta (generalmente entre $65-75).
ASPCA Poison Control: (888) 426-4435
365 días al año, 24/7
Línea de ayuda de envenenamiento para mascotas: (855) 764-7661
365 días al año, 24/7
– Dr. Ana Valbuena
Why Bringing Your Cat to the Vet Is Like an Alien Abduction…

…And What You Can Do to Help
After a decade in practice, I’m thankful I’ve only had to go the hospital for a cat bite once. Since then, I’ve gained a lot of experience and understanding of the feline psyche, and my best summation of how cats perceive going to the vet is this: It’s an alien abduction.
Think about it. For the most part, cats live their whole lives in a relatively small area, and an overwhelming majority of them love it that way.
The most important aspect of a cat’s life is their territory (which includes you). Their territory is their world, their home planet.
Most cats rarely travel in cars and only ever see a travel carrier when they are headed to the vet. Imagine, you’re living your life on your home planet, then you are forced into a pod, and thrust into a metal vessel, and taken to a faraway place that smells aseptic and strange. While there, a weird, hairless ape pokes and prods you. Then, you are thrust back into the pod, whisked home, and your owner acts like nothing happened.
I’m honestly surprised more cats haven’t attacked me. I’d like to think I’d put up a fight too, if I was abducted by aliens. However, maybe if they had a nice spread out and some calming aromatherapy, I’d be amenable to some polite questioning.
Making the Vet Visit as Low Stress as Possible
So that’s what we try to do for your feline family members. Here at Medical District Veterinary Clinic, we are Fear Free Certified. This means all the staff members here have taken training in how to make the veterinary experience as low stress as possible.
We have cat treats at the ready, Feliway spray aplenty, and a separate cat area. We also have gone to great lengths to learn how cats think and how to read their body language. We understand what’s important to them.
Cats often get a bad rap. People think that cats are aloof and don’t care about anything, but cats care about everything! Please know that we are doing our best to be peaceful and compassionate alien overlords.
Try This at Home
There are a few things you can do as well to make the trip to the vet a little less stressful. The first is getting your furry felines accustomed to the carriers you use to take them places.
Just bringing the carrier out before a vet visit can be a trigger. If you’re able to leave the carriers out, put your cat’s favorite treats or toys in there. This small step can help greatly to reduce your cat’s aversion to the carrier.
You can also try using products like Feliway spray, Composure treats for cats, or Rescue Remedy. If you think your kitty needs something stronger, talk to us and we may prescribe medications to help make the visit less stressful. For more information about eliminating the stress in your cat’s life, The Ohio State University Veterinary College has a wonderful site call the Indoor Pet Initiative with information about dogs and cats.
So remember, next time Fluffy’s wellness exam comes around, you may be envisioning All Creatures Great and Small, but they may be thinking more Schwarzenegger in Predator.
—Alyssa Kritzman, DVM
FAQs on CCL: Cranial Cruciate Ligament Injuries in Dogs

I frequently speak with pet owners whose dog has a suspected CCL injury. Here are the most common questions these owners have.
What is a CCL (cranial cruciate ligament)?
The cranial cruciate ligament is a ligament inside the knee of dogs that provides stability of the knee when a dog runs and walks. This ligament is very similar to the anterior cruciate ligament (known as the ACL) in people. These ligaments in dogs and people have nearly identical anatomy but different names because dogs walk on four limbs and people on two. CCL ligaments are only found in dogs’ back legs.
How is an injury to this ligament diagnosed?
In most cases, dogs present to the veterinary clinic with a back leg lameness or limp. Veterinarians will examine the dog, trying to isolate the source of pain. Veterinarians use two techniques to test the stability of the knee: cranial tibial thrust and cranial drawer. If there is thrust and/or drawer present in a dog’s knee, this indicates there is a CCL injury. X-rays are often recommended to help rule out any other causes of pain or lameness, but the ligament itself cannot be seen on x-rays. There are some x-ray findings that make veterinarians suspicious of underlying CCL injury, but true diagnosis is made from physical exam and laxity in the knee joint.
How did this rupture happen?
In dogs, cranial cruciate ligament injury and/or rupture is thought to be due to degeneration of the ligament over time. Unlike people, where a traumatic injury – often sports-related – causes ACL injuries, in dogs the cause is usually degeneration, which leads to injury or even rupture through normal activity. Although a traumatic injury can cause a CCL rupture in dogs, it is less common.
What can we do to help our dog feel better?
When a dog experiences a CCL injury, anti-inflammatory pain medications and rest are recommended. Human pain medications are not safe for dogs, so be sure to consult your veterinarian to discuss appropriate medications for your dog. In addition to rest and medications, surgery is the gold standard for treatment of a CCL injury. Various surgical techniques are available, and your veterinarian will discuss the best option for your dog.
How much does surgery cost?
I recommend that owners see a board-certified surgeon for their pet’s orthopedic surgery. These veterinarians have had additional training to specialize in advanced surgical techniques. As previously mentioned, there are multiple different surgical stabilization techniques for CCL injuries. The most-performed technique in the Chicago area is the Tibial Plateau Leveling Osteotomy (TPLO). These procedures cost between $4,000 to $6,000 in Chicagoland.
Can we use a brace like in humans?
Unfortunately, braces and/or wraps are typically not beneficial in dogs. This is because dogs walk on their tiptoes, so their knee is always bent. (Try it: If you stand on your tiptoes, your knee will be bent too). We humans walk flat-footed, so our weight can transfer from our hip to heel. Since this weight transfer cannot occur in dogs, braces are ineffective.
What if surgery is not an option?
In many cases, surgery is not financially feasible, or it may not be in the best interest of the dog due to other underlying health issues. In these cases, I recommend multi-modal therapy. This includes strict rest for 4 to 8 weeks, long-term non-steroidal anti-inflammatories (NSAIDs), high-quality omega-3 supplements, and glucosamine/chondroitin supplements, along with weight loss. After the period of rest, physical therapy can be very beneficial as well.
With time, the knee will stabilize, but with the stabilization comes more arthritis formation. The body develops arthritis to try to stabilize the knee joint. Surgery on the knee reduces instability, so the body does not form as much arthritis in that joint. However, even with arthritis, dogs are able to compensate well. Many dogs do well without surgery, although the injured leg may always cause some discomfort. The dogs that typically do not do well without surgery are very large dogs that already have joint disease, such as advanced hip dysplasia.
One exception to the surgery rule is toy breed dogs and cats. We do not commonly see CCL injuries in these pets, but when we do, they typically do really well with cage rest and medications and surgery is not often needed.
What about the other leg?
Unfortunately, over 50% of dogs will rupture their other CCL within a year of the first rupture. This can be explained by the fact that both ligaments are typically degenerating at a similar rate. I like to always warn owners of this because they may be faced with the decision to pursue surgery again soon.
How can we prevent a CCL injury?
Unfortunately, there seems to be a hereditary component. We do not have a good method of determining which dogs that will have CCL injuries in their life. However, maintaining an ideal weight is key to joint health. I would also recommend considering pet insurance prior to any issues. Insurance does not cover pre-existing conditions, so don’t wait until your pet starts limping. I have seen CCL injuries in dogs as young as 6 months old, but most commonly we see them in medium to large breed, active, overweight dogs aged 2 to 6 years old.
Dr. Drew Sullivan
