Our Blog
La Importancia de los Cultivos de Orina en las Infecciones del Tracto Urinario y Consejos Para Prevenir

Las infecciones del tracto urinario (ITU) son una preocupación común en la medicina veterinaria. Estas infecciones pueden causar una serie de síntomas incómodos y potencialmente graves en nuestras mascotas, incluyendo micción dolorosa, aumento de la frecuencia urinaria, y en casos más severos, fiebre y letargo. Aunque los síntomas pueden sugerir una ITU, otras condiciones, como las piedras en la vejiga o las enfermedades renales, pueden presentar síntomas similares. Por eso es crucial que la mascota sea examinada por su veterinario antes de empezar tratamiento.
Para diagnosticar y tratar eficazmente una ITU, uno de los pasos más críticos es realizar un cultivo de orine. Una vez que se identifica la bacteria causante, el cultivo de orine también suministra información crucial sobre qué antibióticos serán efectivos. Algunas bacterias pueden ser resistentes a ciertos antibióticos, y el uso de un medicamento ineficaz no solo retrasa la recuperación, sino que también puede contribuir a la resistencia bacteriana.
Infecciones Crónicas o Recurrentes
En algunos casos, las infecciones urinarias pueden ser crónicas o recurrentes. Esto es especialmente común en mascotas con condiciones que predisponen a las infecciones, como la diabetes o las anormalidades anatómicas del tracto urinario.
Para estos animales, se recomienda evaluación por un veterinario por lo menos dos veces al año. Es aun mas importante los cultivos de orine regulares para estos pacientes para monitorear la efectividad del tratamiento y ajustar la terapia según sea necesario. Esta vigilancia continua ayuda a prevenir complicaciones graves y a mantener la salud a largo plazo de la mascota.
Consejos Para Prevenir ITUs
- Hidratación Adecuada: asegúrese que su mascota siempre tenga acceso a agua fresca y limpia. Nunca debe prevenir que su mascota tome más agua. Hidratación adecuada ayuda a eliminar las bacterias del tracto urinario.
- Descansos Regulares para Orinar: Permite que tu perro orine con frecuencia. Retener la orina durante períodos prolongados puede promover el crecimiento bacteriano. La regla de las cajas de arena para los gatos es una caja por gato más una extra.
- Dieta Adecuada: Una dieta equilibrada es importante para mantener la salud general y fortalecer el sistema inmunológico. Su veterinario puede aconsejar en una dieta para su mascota.
- Higiene: Mantén limpia el área genital de tu perro. Los gatos son muy buenos en mantener su propria limpieza, pero pueden tener dificultades si están sobrepeso o si tiene artritis. Recorta el pelo alrededor del área genital para evitar que las bacterias se adhieran al pelaje. Limpia la parte trasera y luego la vulva después de ir al baño.
- Mantener un Peso Saludable: Las mascotas con sobrepeso son más propensos a las ITUs. El ejercicio regular y una dieta adecuada pueden ayudar a mantener un peso saludable.
- Monitorear los Síntomas: Observa los signos de una ITU, como micción frecuente, esfuerzo, sangre en la orina o comportamiento inusual. La detección y el tratamiento tempranos pueden prevenir problemas más graves.
- Evitar el Estrés: El estrés puede debilitar el sistema inmunológico. Trata de minimizar las situaciones estresantes y proporciona un ambiente calmado y estable.
Y como nota final, vamos a estar cerrados el 19 de junio por Juneteenth. Regresamos de 7 am – 7 pm el próximo día.
– Ana Valbuena (she/her/ella), DVM
Urinary Tract Infections: Why We Culture, Tips for Prevention

Urinary tract infections (UTIs) are a common concern in veterinary medicine. These infections can cause a range of uncomfortable and potentially serious symptoms in our pets, including painful urination, increased urinary frequency, and in more severe cases, fever and lethargy. Although symptoms may suggest a UTI, other conditions, such as bladder stones or kidney disease, can present similar symptoms. This is why it is crucial that the pet is examined by a veterinarian before starting treatment.
To diagnose and effectively treat a UTI, one of the most critical steps is performing a urine culture. Once the causative bacteria are identified, the urine culture also provides crucial information about which antibiotics will be effective. Some bacteria may be resistant to certain antibiotics, and using an ineffective medication not only delays recovery but can also contribute to bacterial resistance.
Chronic or Recurrent Infections
In some cases, urinary infections can be chronic or recurrent. This is especially common in pets with conditions that predispose them to infections, such as diabetes or anatomical abnormalities of the urinary tract.
For these animals, evaluation by a veterinarian at least twice a year is recommended. Regular urine cultures are even more important for these patients to monitor treatment effectiveness and adjust therapy as needed. This continuous monitoring helps prevent serious complications and maintain the long-term health of the pet.
Tips for Preventing UTIs
- Adequate Hydration: Ensure your pet always has access to fresh, clean water. Never prevent your pet from drinking more water. Adequate hydration helps flush out bacteria from the urinary tract.
- Regular Bathroom Breaks: Allow your dog to urinate frequently. Holding urine for prolonged periods can promote bacterial growth. The rule for litter boxes for cats is one box per cat plus one extra.
- Proper Diet: A balanced diet is important to maintain overall health and strengthen the immune system. Your veterinarian can advise on a diet for your pet.
- Hygiene: Keep your dog’s genital area clean. Cats are very good at keeping themselves clean, but they may have difficulties if they are overweight or have arthritis. Trim the hair around the genital area to prevent bacteria from clinging to the fur. Wipe the rear and then the vulva after going to the bathroom.
- Maintain a Healthy Weight: Pets that are overweight are more prone to UTIs. Regular exercise and a proper diet can help maintain a healthy weight.
- Monitor Symptoms: Watch for signs of a UTI, such as frequent urination, straining, blood in the urine, or unusual behavior. Early detection and treatment can prevent more serious problems.
- Avoid Stress: Stress can weaken the immune system. Try to minimize stressful situations and provide a calm and stable environment.
And as a final note, we will be closed on June 19 for Juneteenth. We will be back from 7 am to 7 pm the next day.
– Ana Valbuena (she/her/ella), DVM
Why Should You Spay or Neuter Your Dog or Cat?

Ovariohysterectomy (Spay)
Did you know that 25% of female dogs that are not spayed develop mammary tumors? Mammary tumors are commonly diagnosed in older intact female dogs, and the incidence of the development of mammary tumors in dogs is even higher than in humans.
A spay surgery, also called an ovariohysterectomy, involves the removal of the ovaries and uterus in a female dog. Although it is an invasive surgery, it is one of the most common surgeries performed in a general practice veterinary clinic.
There are many benefits to spaying your pet, and the earlier your pet is spayed the better. Complications that may arise during a female dog’s life if she is not spayed include mammary tumors/cancer and pyometra (infection of the uterus).
Additionally, spaying a dog or cat helps reduce pet overpopulation.
Mammary Cancer Risks

As previously mentioned, during a spay the uterus and both ovaries are removed. Ovaries are the female gonads that are responsible for the production of eggs and the female sex hormones, estrogen and progesterone.
Spaying a female dog reduces her risk of developing mammary cancer. If spayed before her first heat cycle, there is almost no risk that she will develop mammary cancer. After she experiences one heat cycle, the risk goes up to 7%. And after more than one heat cycle, the risk goes up to 25%.
Most mammary tumors in dogs are diagnosed between the ages of 9 and 11 years old. Risk of this tumor type is not associated with a specific breed. Small breed dogs, however, appear to be more affected. This suggests a possible genetic component, although one has not yet been identified.
According to information from Cornell University’s Richard P. Riney Canine Health Center, 50% of mammary tumors are malignant. The only way to determine if a tumor is malignant is to remove it and send it to a histopathology laboratory for interpretation.
Mammary Cancer Signs and Diagnostics
Clinical signs of mammary tumors include swollen glands, a painful abdomen, discharge from glands, ulcers near the mammary chain, and lethargy. An easy test that can be performed at most primary care veterinary clinics is called a fine-needle aspirate. This is a non-invasive test that extracts cells from the growth so that a histopathology laboratory can determine if they are cancerous.
A biopsy is a test that is more invasive than a fine-needle aspirate but less invasive than surgical mass removal.
Surgical removal is recommended if mammary cancer is suspected. Diagnostic tests performed before surgery include blood work and chest radiographs to see if the cancer has spread. Treatment ultimately depends on the type of tumor and its behavior.
If you notice any of the clinical signs for mammary cancer in your female dog, please contact your veterinarian.
Pyometra in Dogs
A pyometra is a life-threatening bacterial infection of the uterus that is caused by hormonal changes in an intact female dog. A pyometra is most common in older intact females, but an unspayed dog of any age could get a pyometra. It can occur 1 to 2 months after a heat cycle.
There are two forms of pyometra, closed and open. An open pyometra—the most common form—is when the cervix is open and infection/discharge drains from the vulva. Clinical signs include malodorous discharge from the vulva, lack of appetite, lethargy, vomiting, and drinking an excessive amount of water. Sometimes there are no clinical signs in an open pyometra. Even so, dogs can decline rapidly if not diagnosed early.
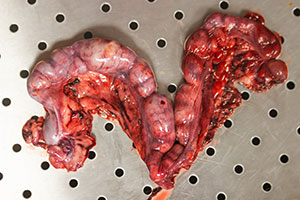
Image by Kseniia from AdobeStock.
With a closed pyometra, the cervix is closed, and the discharge/infection remains inside the uterus. The uterus can rupture in a closed pyometra, and the pet can become septic. This is a medical emergency. Pyometra can be life threatening and the treatment is an emergency spay. Pyometra can be 100% prevented if a female dog is spayed early in life.
Pyometra in Cats
Cats also get pyometra. One major difference in cats, however, is that they rarely appear sick until the very late stages of pyometra. Their abdomen can appear larger and distended due to the size of the discharge-filled uterus. Cats are seasonally polyestrous, meaning that they go into more heat cycles than dogs do, which makes them especially susceptible to getting a pyometra.
As mentioned, an ovariohysterectomy (spay) is a routine procedure performed by many general practice veterinarians. If your female cat or dog is not spayed, please reach out to your local veterinarian to discuss spaying your pet.
Castration (Neuter)
A neuter, also called a castration, involves removing both testicles in a male dog. Testes produce sperm and the male sex hormone testosterone, which is essential for the function of the prostate.
Problems that can arise if a male dog is not neutered include benign prostatic hyperplasia (BPH), prostatitis (infection of the prostate), and testicular cancer. Various studies have shown that neutering a male dog can also help with mounting behavior, inappropriate elimination, and aggression.

Like a spay, a neuter is also a routine procedure and can be performed by most primary care veterinarians. Cats are often neutered under just sedation; the procedure can take less than 5 minutes in cats.
It is highly recommended to neuter your pet after 6 months of age. There is, however, controversy in regard to large breed dogs and bone growth/development. Neutering a large breed dog early has been shown to affect bone growth and lead to joint issues in the future. In a shelter setting, pets are usually neutered at an earlier age to make them more adoptable.
If your male dog/cat is not neutered, please reach out to your local veterinarian to discuss surgery.
Benign Prostatic Hyperplasia (BPH)
Over the course of an intact male dog’s life, the prostate gland gradually enlarges due to the constant hormonal secretion. As an intact male dog ages, the prostate continues to enlarge and that can lead to discomfort/pain. This condition, called BPH, can ultimately interfere with defecation and urination.
Clinical signs of BPH include blood in the urine, difficulty urinating/defecating, and incontinence. An enlarged prostate can often be detected during a rectal exam. These signs however are very nonspecific and can resemble other medical conditions, such as a urinary tract infection, bladder stones, bladder crystals, or bladder tumor.
Neutering a male dog causes the prostate to shrink due to decreased hormonal secretion, which resolves BPH. If a dog has BPH, he will likely need anti-inflammatories and pain medications until surgical removal of the testicles. Ultimately, removing the testicles (neutering) is the treatment of choice.
Testicular Cancer
Testicular tumors are the most common genital tumors found in intact male dogs. Most testicular tumors are malignant, which means they have the potential to spread to other parts of the body.
Testicular tumors usually occur in older dogs, with an average age of 10 years old. The tumors can grow on one or both testicles. Clinical signs include asymmetric testicles, pain near groin, testicular swelling, and visibly larger testicle/testicles. Other signs include poor appetite, weight loss, and lethargy.
Treatment of choice is neutering the pet. Depending on the type of cancer, further treatment such as radiation or chemotherapy might be needed. Diagnostics, including blood work and chest radiographs to check for cancer spread, are performed before surgery.
Neutering your pet eliminates the risk of testicular cancer. If your male dog is intact and you would like to schedule a neuter surgery, please reach out to your veterinarian.
Cystine Crystals/Stones
The amino acid cystine can be excreted in the urine and can lead to the formation of bladder and kidney stones. Although cystine crystals and stones are rare, they are influenced by the presence of sex hormones. These types of crystals and stones are common in intact male dogs and require surgical removal.
Clinical signs may include straining to urinate, blood in the urine, and frequent urination episodes. Due to the anatomical difference in males and females, urinary obstruction is more common in males and it is a medical emergency.
Please reach out to your local veterinarian to further discuss spaying and neutering your pet, as there are many great benefits and various complications can be avoided if performed at an early age.
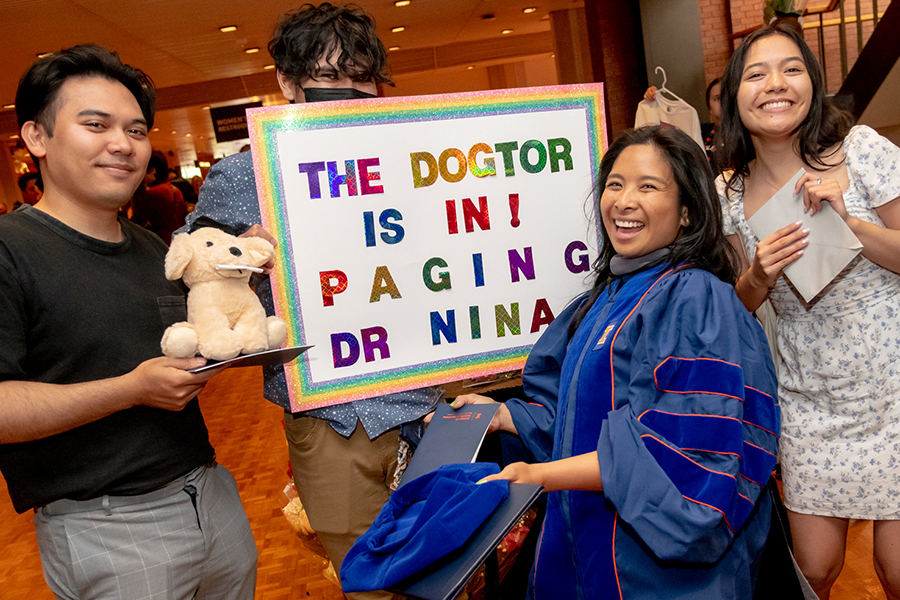
By Dr. Angélica Calderón
Images of Medical District staff and patients by Veronica
Por qué deberías esterilizar y castrar a tu perro/gato?

Ovariohisterectomía (esterilización)
Sabías que el 25% de las perras que no están esterilizadas desarrollan tumores mamarios? Los tumores mamarios se diagnostican comúnmente en perras mayores intactas y la incidencia del desarrollo de tumores mamarios en perros es incluso mayor que en humanos.
Una cirugía de esterilización, también llamada ovariohisterectomía, consiste en la extirpación de los ovarios y el útero de una perra. Aunque se trata de una cirugía invasiva, se realiza con mucha frecuencia y es una de las cirugías más comunes que se realizan en una clínica veterinaria de medicina general. Hay muchos grandes beneficios de esterilizar a su mascota y cuanto antes se esterilice a su mascota, mejor. Pueden surgir varias complicaciones a lo largo de la vida de una perra si no está esterilizada. Esto incluye tumores/cáncer mamario, piometra (infección del útero) y sobrepoblación de perros/gatos si se crían y producen descendencia, especialmente en la comunidad de animales callejeros.
Cáncer de mama
Como se mencionó anteriormente, durante una esterilización se extirpan el útero y ambos ovarios. Los ovarios son las gónadas femeninas que se encargan de la producción de óvulos y de las hormonas sexuales femeninas (estrógeno y progesterona). Esterilizar a una perra puede ayudar en gran medida a reducir la posibilidad de desarrollar cáncer de mama, independientemente de la edad. Sin embargo, hay varios factores a tener en cuenta. Si una perra es esterilizada antes de su primer ciclo de celo, la probabilidad de que desarrolle cáncer de mama es de casi el 0%. Después de experimentar un ciclo de celo, ese número sube al 7%. Si una perra experimenta más de un ciclo de celo, el número sube al 25%. La mayoría de los tumores mamarios se diagnostican entre los 9 y los 11 años de edad. No hay predilección por la raza, sin embargo, los perros de razas pequeñas parecen estar más afectados, lo que sugiere un posible componente genético. Sin embargo, aún no se ha identificado una mutación genética. Según el Centro de Salud Canina Richard P. Riney de Cornell, el 50% de los tumores mamarios son malignos y la única forma de determinar si un tumor es maligno es extirparlo y enviarlo para su interpretación histopatológica.
Los signos clínicos de los tumores mamarios incluyen glándulas inflamadas, abdomen doloroso, secreción de glándulas, úlceras cerca de la cadena mamaria y letargo. Una prueba fácil que se puede realizar en la mayoría de las clínicas veterinarias de atención primaria se llama aspirado con aguja fina. Se trata de una prueba no invasiva que se realiza habitualmente para evaluar el tipo de células presentes en el crecimiento. Estas muestras se envían para su interpretación histopatológica para evaluar si el crecimiento es canceroso. Otra prueba que se puede realizar es una biopsia, que es más invasiva que un aspirado con aguja fina, pero menos invasiva que la extirpación quirúrgica de masas. La extirpación quirúrgica es la recomendación de elección si se sospecha cáncer de mama. Se realizan varios diagnósticos antes de la cirugía; Estos incluyen análisis de sangre básicos, así como radiografías de tórax para evaluar la metástasis (diseminación). El tratamiento depende, en última instancia, del tipo de tumor y de su comportamiento. Si se observa alguno de los signos clínicos mencionados anteriormente en su perra intacta, comuníquese con su veterinario local para que se realicen los siguientes pasos apropiados.
Piometra

Una piometra es una infección bacteriana del útero potencialmente mortal causada por cambios hormonales en una perra intacta. Esto es más común en hembras mayores intactas debido a los diversos ciclos de celo de que han pasado, sin embargo, una perra intacta de cualquier edad es susceptible de contraer una piometra. Esto puede ocurrir de 1 a 2 meses después de un ciclo de celo y los signos clínicos incluyen secreción maloliente de la vulva, falta de apetito, letargo, vómitos y beber una cantidad excesiva de agua. Hay dos formas de piometra, cerrada y abierta. A veces, no hay signos clínicos en una piometra abierta, sin embargo, las perras pueden decaer rápidamente si no se diagnostican a tiempo. Una piometra abierta es cuando el cuello uterino está abierto y la infección/secreción drena fuera del cuerpo fuera de la vulva. Esta es la forma más común. Con una piometra cerrada, el cuello uterino se cierra y la secreción/infección permanece dentro del cuerpo en el útero. De esta forma, el útero puede romperse y la mascota puede volverse séptica. Esto es una emergencia médica. Una piometra puede poner en peligro la vida y el tratamiento para esto es una esterilización de emergencia. Esto se puede prevenir al 100% si una perra es esterilizada a una edad temprana.
Lo mismo se aplica a las gatas, sin embargo, una diferencia importante en las gatas es que rara vez parecen enfermas hasta las últimas etapas de la piometra. Su abdomen puede parecer más grande y distendido debido al tamaño del útero lleno de secreción. Las gatas son estacionalmente poliestroles, lo que significa que entran en más ciclos de celo que las perras, lo que los hace especialmente susceptibles a contraer una piometra.
Como se mencionó, una ovariohisterectomía (esterilización) es un procedimiento de rutina realizado por muchos veterinarios de práctica general. Si tu gata o perra no está esterilizada, comunícate con tu veterinario local para hablar sobre la esterilización de tu mascota.
Castración
Una castración consiste en extirpar ambos testículos en un perro macho. Los testículos producen espermatozoides y las hormonas sexuales masculinas (testosterona), que son esenciales para la función de la próstata. Pueden surgir varios problemas si un perro macho no está castrado. Esto incluye la hiperplasia prostática benigna (HPB), la prostatitis (infección de la próstata) y el cáncer testicular. Se han realizado varios estudios que muestran que la castración de un perro macho también puede ayudar con el comportamiento de montaje, la eliminación inapropiada y la agresión. Al igual que una esterilización, una castración también es un procedimiento de rutina y puede ser realizado por la mayoría de los veterinarios de atención primaria. Los gatos a menudo son castrados bajo sedación y el procedimiento real puede tomar tan solo menos de 5 minutos en gatos. Se recomienda encarecidamente castrar a su mascota después de los 6 meses de edad, sin embargo, existe controversia con respecto a los perros de razas grandes y el crecimiento/desarrollo óseo. Se ha demostrado que la castración temprana de un perro de raza grande afecta el crecimiento óseo y provoca problemas en las articulaciones en el futuro. En un refugio, las mascotas suelen ser castradas a una edad más temprana debido a fines de adopción.
HPB (Hiperplasia Prostática Benigna)

A lo largo de la vida de un perro macho intacto, la glándula prostática se agranda gradualmente debido a la constante secreción hormonal. A medida que un perro macho intacto envejece, la próstata continúa agrandándose y eso puede provocar molestias o dolor. Esto se denomina HPB (hiperplasia prostática benigna) y, en última instancia, puede interferir con la defecación y el orine a medida que la próstata continúa agrandándose.
Los signos clínicos de la HPB incluyen sangre en la orina, dificultad para orinar/defecar e incontinencia. Sin embargo, estos signos son muy inespecíficos y pueden parecerse a otras afecciones médicas como una infección del tracto urinario, cálculos en la vejiga, cristales en la vejiga o tumor en la vejiga. La castración de un perro macho hace que la próstata se encoja debido a la disminución de la secreción hormonal cuando se extirpan los testículos, lo que en última instancia previene la HPB. Si un perro tiene HPB, es probable que necesite antiinflamatorios y analgésicos. La extirpación total de los testículos (castración) es el tratamiento de elección.
Cáncer testicular
Los tumores testiculares son los tumores genitales más comunes que se encuentran en perros machos intactos. La mayoría de los tumores testiculares son malignos, lo que significa que tienen el potencial de propagarse a otras partes del cuerpo. Los tumores testiculares suelen aparecer en perros mayores con una edad media de 10 años. Pueden crecer en uno o ambos testículos y los signos clínicos incluyen testículos asimétricos, dolor cerca de la ingle, hinchazón testicular y un testículo o testículos visiblemente más grandes. Otros signos incluyen falta de apetito, pérdida de peso y letargo.
El tratamiento de elección es la castración de la mascota. Dependiendo del tipo de cáncer, es posible que se necesite un tratamiento adicional como radiación o quimioterapia. Se realizan varios diagnósticos antes de la cirugía, como radiografías de tórax para evaluar la metástasis (diseminación) y análisis de sangre. Castrar a tu mascota eliminará el riesgo de cáncer testicular. Si tu perro macho está intacto y deseas programar una cirugía de castración, comunícate con tu veterinario.
Cristales de cistina
El aminoácido cistina puede excretarse en la orina y provocar la formación de cálculos en la vejiga y los riñones. Aunque los cristales y cálculos de cistina son raros, están influenciados por la presencia de hormonas sexuales. Este tipo de cristales y piedras son comunes en los perros machos intactos y requieren cirugía.
Los signos clínicos pueden incluir esfuerzo para orinar, sangre en la orina y episodios frecuentes de micción. Debido a la diferencia anatómica en machos y hembras, la obstrucción urinaria es más común en los machos y se trata de una emergencia médica.
Comunícate con tu veterinario local para hablar más sobre la esterilización y castración de tu mascota, ya que hay muchos beneficios y se pueden evitar varias complicaciones si se realiza a una edad temprana.
By Dr. Angélica Calderón
Images of Medical District staff and patients by Veronica
Worms and Fleas and Ticks, Oh My!

Our clinic is switching from Sentinel Spectrum to Interceptor Plus. So what does that mean for your pups?
To say that it can be confusing when it comes to knowing what preventative products your dog needs is a bit of an understatement. Does your pet really need this stuff? Is it just marketing? Is this a Coke vs Pepsi thing, or are there actual differences in these products?
It can be confusing even for us in the field trying to keep up with all the new options. That’s why we at Medical District Veterinary Clinic have curated a few products we believe in, so you don’t have to do all the research.
Here is what we have and why.
| Product Name | Parasites Covered | Pros | Cons |
| Heartworm/Intestinal Parasites | |||
| Heartgard | Heartworm, hookworms, roundworms, whipworms | + Less expensive + Beef flavored soft chew + More palatable | – Does not cover tapeworms |
| Interceptor Plus | Heartworm, hookworms, roundworms, whipworms, tapeworms | + More expansive coverage of intestinal parasites | – Less economical than Heartgard |
| ProHeart 12 | Heartworm (for 1 year), hookworms, roundworms, whipworms | + One-time injection + About the same price as 12 months of Heartgard | – Hookworm, roundworm, and whipworm preventative only lasts for 1 month |
| Simparica Trio | Heartworm, hookworms, roundworms, whipworms, fleas, ticks | + Product closest to being an “all-in-one” + Less expensive than purchasing Heartgard and NexGard together | – Does not cover tapeworms |
| Fleas/Ticks | |||
| Frontline Gold | Fleas, ticks | + More economical than oral products + Topical (no concern with food sensitivities) | – Less effective against ticks than oral preventatives – Topical (can be messy; need to keep pet away from children for a few hours after application) |
| NexGard | Fleas and ticks | + Works within hours + Soft chew | – More expensive than topicals |
| Simparica Trio | See above | See above | See above |
So which products should you use for your dog? We recommend that all dogs are covered for heartworm, fleas, and ticks year-round, so here are a few combinations to consider:
- Want the simplest way to have your pet covered? Simparica Trio
- Want the most comprehensive coverage? NexGard and Interceptor Plus
- Want to avoid any oral medications? Proheart 12 and Frontline Gold
- Want the most economical year-round coverage? Heartgard and Frontline Gold
So why did we make the decision to transition away from Sentinel Spectrum and move to Interceptor Plus? Mostly to help keep costs down for you. Interceptor Plus is less expensive, and there is just a slight difference in that Interceptor Plus does not have Lufenuron, which stops the development of flea eggs. Lufenuron doesn’t kill adult fleas, so we recommend an additional flea preventative anyway.
If you are dead set on keeping your pup on Sentinel Spectrum, not a problem! We are happy to approve a prescription for you, as long as your pet is a current patient of ours and has an up-to-date heartworm test.
– Dr. Alyssa Kritzman
Illustration from AdobeStock by Double Brain
Heart Murmurs in Dogs and Cats

Your veterinarian told you that your pet has a heart murmur, but what does that mean?
A heart murmur is an additional noise heard due to the abnormal flow of blood through the heart’s valves or chambers. This additional noise is then graded on a scale of 1 to 6 based on how loud the heart murmur is. A 1 means the softest and hardest to hear, and a 6 means the loudest.
How loud the heart murmur is does not necessarily correlate to the severity of heart disease. If your pet has a heart murmur, it is not an immediate cause for panic, but rather lets your veterinarian know that more investigation should be done to try and find the cause.
What Causes a Heart Murmur?
There are many causes of heart murmurs. Some heart murmurs are considered “innocent,” also termed “physiologic.” Other heart murmurs are a result of a disease, and these are known as “pathologic.” Pathologic heart murmurs can be caused by a structural problem with the heart or can be caused by disease not related to the heart itself, called functional heart murmurs.
Innocent Heart Murmurs
An innocent heart murmur means there is no heart disease that explains the presence of the heart murmur. In dogs, these murmurs occur most often in puppies. They can occur in cats of any age.
These murmurs are usually very soft. In puppies and kittens, these murmurs usually appear around 6 to 8 weeks of age and should go away on their own by the age of 4 to 5 months. In adult cats, stress may cause an innocent heart murmur.
Structural Heart Disease
An abnormal defect or structure that disrupts the normal flow of blood leads to structural heart disease. Examples of these include valve disease that causes the valves between the chambers of the heart to not close or open properly, a hole in the heart that causes two chambers or two arteries to be connected when they shouldn’t be, and narrowing or widening of the blood vessels.
Functional Heart Murmurs
Heart murmurs can also be caused by disease outside of the heart, or extra-cardiac disease. There are many causes of functional heart murmurs, including anemia (low levels of red blood cells), fever, pregnancy, infection, obesity, being significantly underweight, and hypoproteinemia (low protein levels in the blood).
Signs, Diagnostics, and Treatment
In some cases, your pet may not be experiencing any signs of having a heart murmur. In others, you may have noticed signs of poor appetite, exercise intolerance, trouble breathing or fast breathing when resting or sleeping, collapse or fainting, weight loss, coughing, pale gums, and weakness.
If your pet is found to have a heart murmur, your veterinarian will discuss additional testing that may be beneficial in finding the cause of the heart murmur and to determine the severity of the condition causing the murmur. Diagnostics that may be suggested include bloodwork, chest X-rays, and blood pressure testing.
Your veterinarian will likely suggest referral to a veterinary cardiologist or an imaging center for an echocardiogram. An echocardiogram is an ultrasound of the heart to get an idea of what the heart looks like and how it is functioning in real time. More specifically, an echocardiogram will provide information about the shape, size, and function of the heart’s four chambers, valves, and other surrounding structures.
Together, these diagnostics will provide your pet’s veterinarian with the information needed to determine what treatment and medication, if needed, will be necessary to help your pet live a longer, happy life.
By Dr. Jeanette Barragan
Illustration from photo by Gajus
La Importancia de la Diversidad en la Medicina Veterinaria

En honor al Mes de La Historia Afroamericana, profundizaremos en por qué la diversidad es importante en la medicina veterinaria.
La diversidad en la medicina veterinaria no es solo un imperativo moral; es una necesidad para el avance del campo y la provisión de atención equitativa a todos los animales. Sin embargo, a pesar del reconocimiento creciente de su importancia, persisten disparidades en la representación de grupos minoritarios dentro de los programas veterinarios.
Mejor Acceso a la Atención
Las comunidades minoritarias a menudo enfrentan barreras para acceder a la atención veterinaria, incluyendo factores socioeconómicos, lenguaje, diferencias culturales y ubicación geográfica. Con solo 1.3% de veterinarios afroamericanos/negros y 7.9% hispanos/latines reportados en 2023, al aumentar la diversidad dentro de la profesión veterinaria, podemos comprender y abordar mejor las necesidades únicas de estas comunidades, asegurando que todos los animales reciban la atención que merecen.
Innovación y Resolución de Problemas
Los equipos diversos son más hábiles para resolver problemas e innovar debido a la variedad de perspectivas y enfoques que aportan. En la medicina veterinaria, esta diversidad de pensamiento puede llevar a soluciones creativas para desafíos complejos, desde la prevención de enfermedades hasta las metodologías de tratamiento.
Representación y Modelos a Seguir
Aumentar la diversidad dentro de los programas veterinarios, sean doctores, enfermeros, asistentes, o personal de recepción, presenta una oportunidad para los grupos subrepresentados modelos a seguir y mentores a quienes pueden relacionarse e inspirarse para emular. Esta representación es esencial para inspirar a las futuras generaciones de profesionales veterinarios diversos y derribar barreras de entrada al campo.
Estadísticas sobre las Tasas de Aceptación para Minorías
Aunque ha habido avances en el aumento de la diversidad dentro de los programas veterinarios, persisten disparidades en las tasas de aceptación para estudiantes de minorías. Según datos recientes:
- Los estudiantes afroamericanos/negros constituyen solo un pequeño porcentaje de los solicitantes y matriculados en escuelas de veterinaria, con tasas de aceptación significativamente más bajas que las de sus contrapartes blancos.
- Los estudiantes hispanos/latines también están subrepresentados en los programas veterinarios, enfrentando barreras como acceso limitado a recursos educativos y limitaciones financieras.
- Los estudiantes indígenas/nativos americanos están entre los grupos más subrepresentados en la medicina veterinaria, con tasas de aceptación muy por debajo del promedio nacional.
A pesar de los esfuerzos para promover la diversidad y la inclusión dentro de la educación veterinaria, estas estadísticas resaltan la necesidad de defensa y acción continuas para abordar barreras sistémicas y aumentar el acceso a programas veterinarios para estudiantes de minorías.
Conclusión
La diversidad no es solo una palabra de moda; es un aspecto fundamental de la medicina veterinaria que enriquece la profesión y mejora la calidad de la atención proporcionada a los animales. Con 25% de grupos subrepresentados componiendo la clase de 2025 en el Colegio de Medicina Veterinaria en la Universidad de Illinois, seguiremos los esfuerzos para aumentar la representación y abordar las disparidades en las tasas de aceptación para minorías. Podemos construir una fuerza laboral veterinaria más inclusiva que refleje la diversidad de las comunidades a las que servimos. Es hora de reconocer la importancia de la diversidad en la medicina veterinaria y tomar medidas significativas hacia la creación de una profesión más equitativa e inclusiva.
—Dr. Ana Valbuena
The Importance of Diversity in Veterinary Medicine
Diversity in veterinary medicine is not just a moral imperative; it’s a necessity for advancing the field and providing equitable care to all animals. However, despite the growing recognition of its importance, disparities persist in the representation of minority groups within veterinary programs.
In honor of Black History Month, we will delve into why diversity is important in veterinary medicine.
Better Access to Care
Minority communities often face barriers to accessing veterinary care, including socioeconomic factors, language barriers, cultural differences, and geographical location. According to the Bureau of Labor Statistics, among all U.S. veterinarians in 2023 only 1.3% are African American/Black veterinarians and 7.9% are Hispanic/Latinx veterinarians. Increasing diversity within the veterinary profession allows us to better understand and address the unique needs of these communities, ensuring that all animals receive the care they deserve.
Innovation and Problem Solving
Diverse teams are more adept at problem-solving and innovation due to the variety of perspectives and approaches they bring. In veterinary medicine, this diversity of thought can lead to creative solutions for complex challenges, from disease prevention to treatment methodologies.
Representation and Role Models
Increasing diversity within veterinary programs, whether doctors, nurses, assistants, or reception staff, provides an opportunity for underrepresented groups to find role models and mentors they can relate to and aspire to emulate. This representation is essential for inspiring future generations of diverse veterinary professionals and breaking down barriers to entry into the field.
Statistics on Acceptance Rates for Minorities
Although there have been advances in increasing diversity within veterinary programs, disparities persist in acceptance rates for minority students. According to recent data:
- African American/Black students make up only a small percentage of applicants and enrollees in veterinary schools, with significantly lower acceptance rates than their white counterparts.
- Hispanic/Latinx students are also underrepresented in veterinary programs, facing barriers such as limited access to educational resources and financial constraints.
- Indigenous/Native American students are among the most underrepresented groups in veterinary medicine, with acceptance rates far below the national average.
Despite efforts to promote diversity and inclusion within veterinary education, these statistics highlight the need for continued advocacy and action to address systemic barriers and increase access to veterinary programs for minority students.
Conclusion
Diversity is not just a trend; it’s a fundamental aspect of veterinary medicine that enriches the profession and improves the quality of care provided to animals. For the past four years, the incoming class of students at the College of Veterinary Medicine at the University of Illinois has been made up of one-quarter students from underrepresented groups. We will continue efforts to increase representation and address disparities in acceptance rates for minorities. We can build a more inclusive veterinary workforce that reflects the diversity of the communities we serve. It’s time to recognize the importance of diversity in veterinary medicine and take meaningful steps toward creating a more equitable and inclusive profession.
—Dr. Ana Valbuena
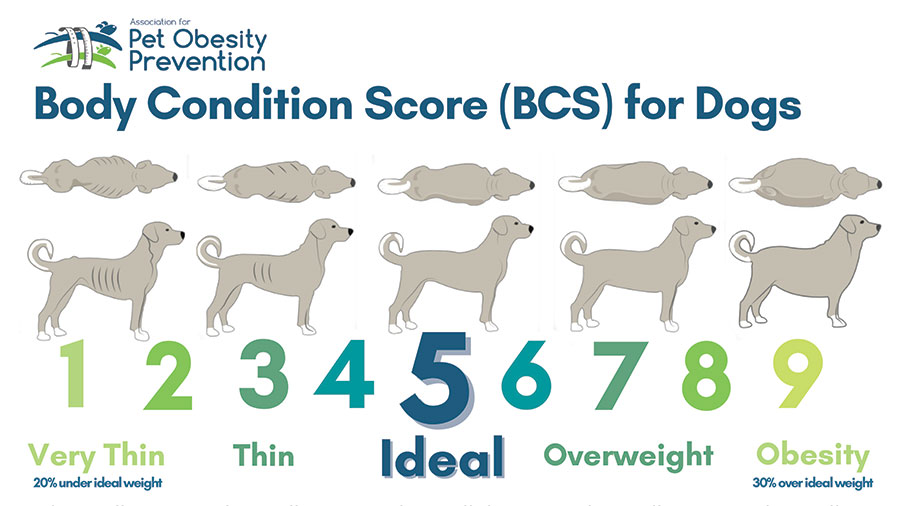
New Year’s Resolution: No Overweight Pets

With the start of the new year, you might have noticed an increase in the number of gym memberships and more people waiting in line to use the elliptical. If you’ve also noticed that your pet at home has packed on a couple of extra holiday pounds, now would be a perfect time to start considering some weight loss for your pet. Increased weight can lead to obesity, and various negative health conditions can follow.
How Do I Know If My Pet Is Overweight?
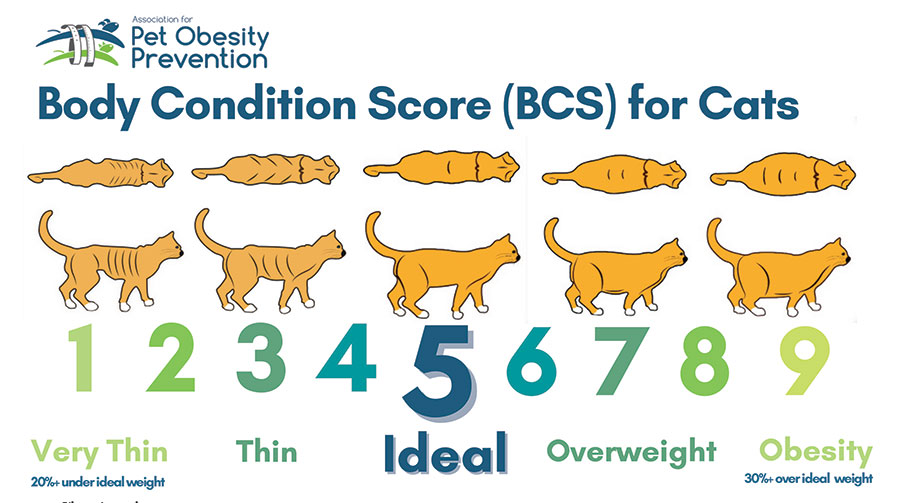
Pets are given a body condition score (BCS) to determine if they are overweight, underweight, or at an ideal body weight. BCS is determined not only by the number on the scale and physical appearance, but also fat deposits felt by your veterinarian during the exam along with amount of muscle mass. Below are charts from the Association for Pet Obesity Prevention that illustrate body condition scores for dogs and cats. Please reach out to your local veterinarian if you would like to know if your pet is overweight.
- Ribs visible from a distance under shorthair, no palpable body fat
- Ribs visible under shorthair, no palpable fat
- Ribs may be visible under shorthair, no palpable fat
- Ribs minimally visible, easy to palpate with minimal fat cover
- Ribs not visible, easy to palpate with minimal fat covering
- Ribs palpable under mild fat covering
- Ribs palpable with difficulty under moderate fat covering. Mild fat deposits over lumbar area and tail base
- Ribs palpable only with significant pressure under marked fat deposits. Moderate fat deposits over lumbar area and tail base
- Ribs not palpable under marked fat deposits. Marked fat deposit over spine including the neck and tail base
What Are the Health Risks?
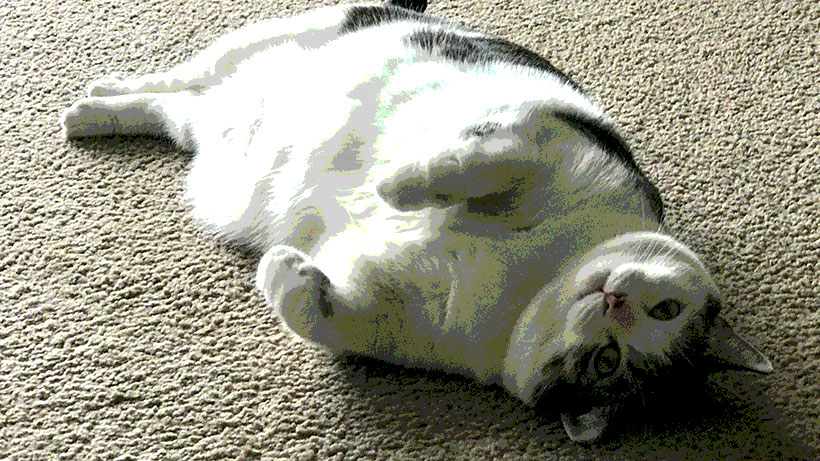
Obesity is associated with many negative health conditions. Such conditions include joint disease and osteoarthritis, heart disease, respiratory distress, decreased grooming in cats, diabetes mellitus, increased anesthetic risk, and ultimately a decreased lifespan.
Joint Disease and Osteoarthritis: Extra weight adds extra pressure and stress on joints, which can lead to early joint degeneration and decreased mobility. This, in turn, can exacerbate obesity. In a patient undergoing a weight loss journey, adding joint supplements can help strengthen joints, which may increase mobility and comfort, ultimately helping with weight loss.
Diabetes Mellitus: Extra body fat can lead to insulin resistance. Weight loss can help decrease a cat’s risk for the development of diabetes mellitus. According to a study at Cornell University College of Veterinary Medicine, obese cats are four times more likely to develop diabetes than are cats with an ideal BCS.
Heart Disease: Although fat is relatively nonvascular tissue, it still requires blood flow, which leads to an increase in circulatory volume and cardiac output, ultimately resulting in hypertension. Compared to dogs with an ideal body weight, obese dogs develop negative changes to the overall structure and function of their heart.
Why Do Pets Become Overweight?
Well, we are the culprits. Overfeeding, lack of exercise, and too many treats can lead to obesity in pets. Various endocrine diseases are associated with obesity, such as Cushing’s disease and hypOthyroidism in dogs. In cats, weight loss and low BCS are commonly associated with hypERthyroidism.
What Do I Do If My Pet Is Overweight?
Weight loss can be a hard, slow process. It takes much time and patience. When your veterinary team works with you and provides the right tools, we can achieve a healthy weight for your pet.
There are many dietary changes that can be done in order to achieve weight loss in your pet. A great start is checking out the Pet Nutrition Alliance website. When you enter your dog’s current weight and body condition score, this website calculates a calorie count for you. It is important to account for all food AND treats using this calorie count. Please reach out to your local veterinarian if you would like to know your pets BCS.
There are several over-the-counter options as well as prescription diets that can be given to your pet for weight loss. When feeding in cups, it is important to use an actual measuring cup to avoid overfeeding/underfeeding. Calories per cup can vary, so please check the back of the bag for an accurate calorie measurement of how many cups your pet should be eating. Healthy, low-calorie fruits and vegetables such as apple slices, carrots, celery, and cucumber can be used as treats. Please avoid grapes, raisins, onion, garlic, and avocados, which can be highly toxic to pets.
Exercise is a very important component in order to achieve weight loss. Therefore, adding more play time, frequent walks, and possibly even a kitty treadmill can help achieve your pet’s weight loss goals. Frequent weigh-ins are also a very important component for weight loss to track the progression of your pet’s weight.
If you suspect that your pet is overweight, please reach out to your primary care veterinarian to you can discuss the best option for your pet.
From ‘Fat Vincent’ to ‘Skinny Vinny’
In 2016, a 7-year-old obese dachshund named Vincent was surrendered to an animal shelter in Houston, Texas, after his owner died. He weighed 38 pounds. Thanks to the help of K-9 Angels Rescue, he was able to lose over half of his body weight and was renamed Skinny Vinny. He weighed in at 17 pounds after an 8-month weight-loss journey.
By Dr. Angélica Calderón
Dog image: VinnieRattolle, CC BY-SA 4.0, via Wikimedia Commons
Propósitos de Año Nuevo para todos
Con el comienzo del nuevo año, es posible que hayas notado un aumento en el número de membresías en gimnasios y más personas esperando en fila para usar la máquina elíptica. Ahora, si ha notado que su mascota en casa subio un par de kilos de más durante las vacaciones, entonces sería un momento perfecto para comenzar a considerar perder algo de peso; ya que el aumento de peso puede provocar obesidad y pueden producirse diversas condiciones negativas de salud.
¿Cómo puedo saber si mi mascota tiene sobrepeso?
A las mascotas se les asigna una puntuación de condición corporal (también conocida como BCS) para determinar si tienen sobrepeso, bajo peso o si tienen un peso corporal ideal. Comuníquese con su veterinario local si desea saber si su mascota tiene sobrepeso.
A continuación se muestran gráficos de la Asociación para la Prevención de la Obesidad de las Mascotas que ilustran las puntuaciones de condición corporal de perros y gatos. Comuníquese con su veterinario local si desea saber si su mascota tiene sobrepeso.
- Costillas visibles desde lejos debajo del pelo corto, sin grasa corporal palpable
- Costillas visibles debajo del pelo corto, sin grasa palpable
- Las costillas pueden ser visibles debajo del pelo corto, no se palpa grasa
- Costillas mínimamente visibles, fáciles de palpar con mínima cobertura de grasa
- Costillas no visibles, fáciles de palpar con una cobertura mínima de grasa
- Costillas palpables bajo una leve capa de grasa
- Costillas palpables con dificultad bajo una cubierta grasa moderada. Depósitos leves de grasa sobre la zona lumbar y la base de la cola.
- Costillas palpables sólo con una presión significativa bajo depósitos de grasa marcados. Depósitos moderados de grasa sobre la zona lumbar y la base de la cola.
- Costillas no palpables bajo depósitos de grasa marcados. Depósito de grasa marcado sobre la columna, incluido el cuello y la base de la cola.
¿Cuales son los riesgos para la salud?
La obesidad está asociada con muchas condiciones de salud negativas. Dichas afecciones incluyen enfermedades como osteoartritis, enfermedades cardíacas, dificultad respiratoria, disminución del aseo en los gatos, diabetes mellitus, mayor riesgo anestésico, y en casos graves menos tiempo de vida.
Enfermedades de osteoartritis: El peso extra añade presión y estrés adicionales a las articulaciones, lo que puede provocar una degeneración temprana de los huesos y una disminución de la movilidad, lo que a su vez puede exacerbar la obesidad. En un paciente que está pasando por un proceso de pérdida de peso, agregar suplementos para los huesos puede ayudar a fortalecer los huesos, lo que puede conducir a una mayor movilidad y mayor comodidad.
Diabetes mellitus: El exceso de grasa corporal puede provocar resistencia a la insulina y la pérdida de peso puede ayudar a disminuir el riesgo de que un gato desarrolle diabetes mellitus. Según un estudio de la Facultad de Medicina Veterinaria de la Universidad de Cornell, los gatos obesos tienen cuatro veces más probabilidades de desarrollar diabetes que un gato con un BCS ideal.
Enfermedad cardíaca: Aunque la grasa es un tejido relativamente no vascular, aún requiere perfusión, lo que conduce a un aumento en el volumen circulatorio y el gasto cardíaco, lo que puede resultar en hipertensión. En comparación con los perros con un peso ideal, los perros obesos tienen varios cambios en la estructura y función general de su corazón.
¿Por qué las mascotas tienen sobrepeso?
Bueno, nosotros somos los culpables. La sobrealimentación, la falta de ejercicio y demasiados premios pueden provocar obesidad en las mascotas. Varias enfermedades endocrinas están asociadas con la obesidad, como la enfermedad de Cushing y el hipotiroidismo en perros, mientras que la pérdida de peso y un nivel bajo de BCS pueden estar asociados con el hipertiroidismo en los gatos.
¿Qué hago si mi mascota tiene sobrepeso?
La pérdida de peso puede ser un proceso lento y difícil y requiere mucho tiempo y paciencia. Somos un equipo pero con las herramientas adecuadas podemos lograr un peso saludable para tu mascota.
Hay muchos cambios en la dieta que se pueden realizar para lograr la pérdida de peso de su mascota. Un buen comienzo es visitar el sitio web de Pet Nutrition Alliance. Este sitio web le permite ingresar el peso actual de su perro junto con su puntuación de condiciones corporales. Se calcula un recuento de calorías. Es importante tener en cuenta todos los alimentos y premios utilizando este recuento de calorías.
Hay varias opciones de venta libre, así como dietas recetadas que se pueden administrar a su mascota para bajar de peso. Varias marcas de alimentos de venta libre tienen una fórmula “baja en calorías” o de “peso perfecto”. Al alimentar en tazas, es importante utilizar una taza medidora para evitar la sobrealimentación o la subalimentación. Las calorías por taza varían, así que revise la parte posterior de la bolsa de comida para obtener una medida precisa de cuánto debe comer su mascota. Se pueden utilizar frutas y verduras saludables bajas en calorías como premio. Varias opciones incluyen rodajas de manzana, zanahorias, apio y pepino. Evite las uvas, las pasas, la cebolla, el ajo y los aguacates, ya que pueden ser muy tóxicos.
El ejercicio es un componente muy importante para lograr la pérdida de peso. Por lo tanto, agregar más tiempo de juego, caminatas frecuentes y posiblemente incluso una cinta de correr para gatos puede ayudar a lograr los objetivos de pérdida de peso de su mascota. Los pesajes frecuentes también son un componente muy importante para la pérdida de peso para realizar un seguimiento de la progresión del peso de su mascota.
Si sospecha que su mascota tiene sobrepeso, comuníquese con su veterinario para que pueda analizar la mejor opción para su mascota.
De ‘Fat Vincent’ a ‘Skinny Vinny’
En 2016, un perro salchicha obeso de 7 años llamado Vincent fue entregado a un refugio de animales en Houston, Texas, después del fallecimiento de su dueño. Pesaba 38 libras. Gracias a la ayuda de K-9 Angels Rescue, pudo perder más de la mitad de su peso corporal y pasó a llamarse Skinny Vinny. Pesó 17 libras después de un viaje de pérdida de peso de 8 meses.
By Dr. Angélica Calderón
Cat image: Jami430, CC BY-SA 4.0, via Wikimedia Commons
Mystery Canine Respiratory Illness
Fear of the Unknown, or Fear of Saying ‘I Don’t Know’?

Originally, I was planning to write this blog about the current “mystery illness” that is popping up in random places around the United States. But when I sat down to research what I could, I kept getting stuck on the word “unknown.” It made me think about all that I haven’t figured out myself yet.
“I don’t know” is a phrase that you are likely to hear from me as your pet’s veterinarian. It is a phrase that I used to be terrified of saying when I first started practicing medicine over a decade ago.
I spent a lot of time (most of my 20s) and money (over six figures) learning everything about biology, chemistry, pharmacology, virology, physiology, anatomy (of multiple species, mind you!), really any animal-related “-ology” so I could avoid that very phrase.
Why I Say ‘I Don’t Know’
Now, with years of experience in the field, I frequently say “I don’t know” because I am so acutely aware that figuring out why an animal is sick (we call this a differential diagnosis) is often much harder than just making an animal feel better (we call this empiric therapy).
There are a few reasons why this is so:
- Answers often cost money. Even the best veterinarians can go only so far on a physical exam and asking good questions. Eventually we need test results, but this costs money—your money—and sometimes we don’t need an answer to find the treatment. We want to put your resources to the best use. If we use up the available budget to find answers, that may mean we have fewer resources to provide the care your pet needs.
- Answers often aren’t easy. One of the worst things that has ever happened to any medical professional is the show CSI. They always find the answer in a convenient hour (or 40 minutes if you’re paying for premium streaming). This is just not reality. Yes, sometimes tests to give you a precise answer, but a lot of times testing provides information and clues. Then I use my expensive degree to put all the pieces of the puzzle together.
- Answers often aren’t universal. This is what I mean when I say a pet “hasn’t read the textbook.” The same problem does not always manifest in the same way in every pet. (Not to put all the blame on cats, but it’s usually cats who haven’t read the textbook!) That can mean that even if we think we know what’s going on, we can get curveballs.
I know this may not instill a lot of confidence in what I and my colleagues do, but I say this because I want you to know that getting an answer isn’t my only goal. I want to help you and your pet in the best way possible. Often these goals are at odds with each other.
We Still Don’t Have an Answer
This brings me to the current “crisis” going on in veterinary medicine right now: the mystery respiratory illness that is affecting dogs. We still don’t have an answer as to what it is. It won’t be easy or cheap to figure out, but there are people working on it. As soon as we have verified information, we will let you know.
For now, we’re left with the general guidance of trying to keep your dog away from crowded canine events as much as possible (I will be boarding my own dog over the Christmas because that’s our only option), keeping them away from unhealthy dogs, and keeping up with the recommended respiratory vaccines like distemper, bordetella, and parainfluenza, and, for some dogs, influenza.
It’s hard accepting “we don’t know,” but to tell you anything more than that would be foolish. In all my years of practice, I would much rather say “I don’t know” than “I was wrong.”
—Dr. Alyssa Kritzman
Diabetes in Cats: Prevention and Treatment

Diabetes mellitus is a condition in which the body cannot properly produce or respond to the hormone insulin. Insulin regulates the amount of glucose (sugar) in the bloodstream and delivers glucose to the tissues of the body to use as energy. Diabetes results in elevated levels of glucose in the blood. The most common form of diabetes in cats is type 2 diabetes. In type 2 diabetes, glucose levels are high because cells in the body do not respond appropriately to insulin.
Diabetes is the second most common endocrine disease in cats. (The body’s endocrine system consists of several glands—in the case of diabetes, that gland is the pancreas—that make hormones, which are chemical messengers to control organs throughout the body.)
Cats are typically diagnosed with diabetes between the ages of 10 and 13 years. More cats are acquiring diabetes as the number of overweight or obese cats grows. The average cat that weighs 13 pounds or more has about four times the risk of developing diabetes as a smaller cat. Signs of diabetes can include increased thirst, increased urination, weight loss, and increased appetite.
Diagnosis
When a cat is suspected of having diabetes, a veterinarian will perform blood and urine testing. Diabetes is indicated if blood testing shows an elevated glucose level (hyperglycemia) and urine testing shows evidence of glucose in the urine (glucosuria).
Because stress in cats can lead to both hyperglycemia and glucosuria, another confirmation test called fructosamine is usually done. Fructosamine concentration reflects the average glucose concentration for the past 1 to 2 weeks and is not impacted by stress. If this test comes back as elevated, the diagnosis of diabetes is confirmed.
Treatment
Insulin is the treatment of choice for cats with diabetes. This typically requires twice daily administration. In addition, dietary management can be an important component of managing diabetes in cats. A high-protein/low-carbohydrate diet is recommended. Weight loss is also an important component of diabetic management in overweight cats. Weight loss, if attempted, should ideally be gradual, one-half percent to 1% of total body weight lost per week.

The goals of treatment are to maintain a healthy blood glucose, stop or control unintended weight loss, stop or control increased thirst and urination, and avoid hypoglycemia (low blood glucose).
Unlike dogs, cats can reach diabetic remission; these cats have near-normal blood glucose levels without receiving insulin or other blood-sugar–lowering medication. However, cats in diabetic remission require close monitoring to ensure that they do not relapse. Remission is not achievable in every diabetic cat.
Monitoring
Blood glucose curves are used to monitor response to insulin dosing. If a blood glucose curve is performed at home, pet owners measure the first blood glucose reading before the insulin injection. Then, they test every 2 to 4 hours until the next dose of insulin, depending on the type of insulin used. Performing curves at home eliminates the stress of coming to the clinic, which can affect the accuracy of the testing. Owners may need to perform a blood glucose curve several times to find the right dose for their cat.
One method of measuring glucose is by using a glucose meter calibrated for feline blood, such as a AlphaTRAK3. Another way is by using a continuous glucose monitor, such as a FreeStyle Libre. These monitors can be picked up at a human pharmacy and installed by a veterinarian or veterinary technician. Other important monitoring tests include serial bloodwork and urine testing. Your veterinarian will help determine the frequency at which these tests should be performed.
Monitoring your cat’s level of thirst and urination, weight, and appetite are important throughout treatment. These measures can give clues as to how well the diabetes is being managed. Unfortunately, monitoring response to treatment in diabetic cats can be frequent and expensive.
Complications of Diabetes
One complication of diabetes is diabetic ketoacidosis (DKA). This problem occurs when there is not enough insulin in the body to control the amount of glucose in the blood. DKA happens in uncontrolled diabetics. Without the proper amount of insulin in the body, glucose cannot be used as an energy source. Instead, the body breaks down fat, which produces ketone bodies. With high levels of ketones, the body becomes more acidic, which disrupts fluid and electrolyte balance. Left untreated, the resulting abnormal electrolyte balance may lead to abnormal heart rhythms and muscle function and death. Signs of DKA can include increased thirst or urination, lethargy, weakness, vomiting, increased respiratory rate, decreased appetite, and weight loss.
The other complication is hypoglycemia, or low blood sugar, which may arise when insulin therapy lowers the blood sugar significantly. Signs of hypoglycemia include weakness, lethargy, vomiting, lack of coordination, seizures, and coma. Hypoglycemia can be fatal if left untreated. A diabetic cat that shows any of these signs should be offered its regular food immediately. If the cat does not eat voluntarily, it should be given oral glucose in the form of honey, corn syrup, or dextrose gels and brought to a veterinarian immediately. However, if a cat is seizing or comatose, oral glucose methods should not be attempted.
If you’ve noticed changes to your cat’s eating and drinking habits as well as weight, please have them seen by a veterinarian for additional testing to be done as soon as possible.
By Jeanette Barragan, DVM
¿Qué hacer cuando su gato(a) hace del baño afuera de su caja?

Photo by Luku Muffin on Unsplash
¡Orinar o defecar fuera de la caja de arena puede ser muy frustrante para todos! También puede ser la primera, y a veces la única, señal de que algo anda mal. Se recomienda encarecidamente una visita al veterinario cada vez que haya un comportamiento inusual en nuestras mascotas, particularmente la micción inapropiada. Mientras tanto, considere lo siguiente:
Todos los gatos necesitan satisfacer sus necesidades básicas. Sin embargo, cuando hay varios gatos en el hogar, es particularmente importante asegurarse de que haya muchos recursos en forma de cajas de arena, estaciones de alimentación, espacios verticales, estaciones para dormir, escondites y tazones de agua. El castigo es ineficaz y confuso para los gatos. El entrenamiento basado en recompensas ayuda a mejorar la comunicación al tiempo que proporciona estimulación mental e interacción humana positiva. Los juguetes dispensadores de alimentos y rompecabezas imitan la caza y fomentan la exploración de su ambiente, reduciendo los niveles generales de estrés y satisfaciendo las necesidades básicas.
Los modelos generales que le ayudarán a satisfacer las necesidades básicas de la caja de arena incluyen las siguientes sugerencias:
- Tenga una caja de arena más que gatos para que los gatos más quisquillosos puedan encontrar una caja limpia. ¡La regla es 1 caja de arena por gato más una extra!
- La ubicación importa: los gatos prefieren un área tranquila y aislada, lejos de electrodomésticos ruidosos, hornos, aire acondicionado y áreas de tráfico pesado.
Considere el uso de feromonas como Feliway para reducir el estrés si ha tenido cambios recientes dentro del hogar (nuevo bebé o mascota, mudanza, visitas, etc.) - El tamaño importa: las cajas de arena deben ser al menos 1.5 veces la longitud del cuerpo del gato y aproximadamente 3 veces más anchas que el gato.
¡Considera crear una nueva caja de arena a partir de un contenedor de almacenamiento si no puedes encontrar una lo suficientemente grande! Las cajas de suéteres debajo de la cama son excelentes cajas de arena.(YouTube tiene muchos videos geniales DIY)
El aumento de peso y la obesidad es un gran problema para nuestros amigos felinos. Además de dificultar encontrar una caja lo suficientemente grande, el exceso de grasa afecta negativamente a la salud y la longevidad de un gato. Tienen un mayor riesgo de cáncer, diabetes y problemas cardíacos. También son propensos a la artritis y a una degeneración más rápida de las articulaciones afectadas: ¡puede doler saltar a la caja o adoptar la postura para ir al baño! - Saca la caja varias veces al día.
- Incluso con arenas aglomeradas, deseche la caja al menos una o dos veces por semana.
- Lave la caja semanalmente, enjuague bien y seque al aire para eliminar cualquier olor del agente de limpieza. El agua caliente y el jabón son los mejores para la limpieza.
- No use arena perfumada, revestimientos o aditivos como bicarbonato de sodio.
- Si al gato le gusta cavar, haz que la arena sea profunda. Si el gato sacude la arena de sus patas, haz que la arena sea poco profunda o cambia a un tipo diferente (aserrín granulado, trigo sarraceno, etc.).
- Lavar, enjuagar y secar cualquier área que el gato haya ensuciado fuera de la caja y luego use un buen removedor de olores. Los mejores ayudan a descomponer enzimáticamente los compuestos de la orina y hacen que algunos odorantes sean demasiado pesados para ser inhalados. NO use lejía ni productos pesados similares.
- De todos modos, siga al gato y vea lo que elige, imite esa elección.
Are You Finding Pee or Poop Outside the Litter Box?
Urinating or defecating outside the litter box can be very frustrating for all! It can also be the very first, and sometimes only, sign that something is wrong. A veterinary visit is highly encouraged any time there is unusual behavior in our pets, particularly inappropriate urination.

In the meantime, consider the following:
All cats need their basic needs met. However, when there are multiple cats in the household, it is particularly important to make sure there are plenty of resources in the form of litter boxes, feeding stations, vertical spaces, sleeping stations, hiding areas, and water bowls. Punishment is ineffective and confusing for cats. Reward-based training helps to improve communication while providing mental stimulation and positive human interaction. Food dispensing and puzzle toys mimic hunting and encourage exploration of their environment, reducing overall stress levels and meeting basic needs.
General guidelines that will help you meet the basic litter box needs include the following suggestions.
- Have one more litter box than you have cats so that fussier cats can find a clean box. The rule is 1 litter box per cat plus an extra!
- Location matters: cats prefer a quiet, secluded area away from loud appliances, furnaces, air conditioning, and heavy traffic areas.
Consider using pheromones like Feliway for stress reduction if you have had recent changes within the household (new baby or pet, moving, visits, etc.) - Size matters: litter boxes should be at least 1.5 times the length of the cat’s body and about 3 times as wide as the cat so the cat can move and turn around.
Consider creating a new litter box out of a storage bin if you cannot find one big enough! Underbed sweater boxes make great litter boxes. (YouTube has many great DIY videos.)
Weight gain and obesity is a huge problem for our feline friends. Apart from making it difficult to find a box that is big enough, excess fat negatively impacts a cat’s health and longevity. Heavy cats are at a higher risk for cancer, diabetes, and heart issues. They are also prone to arthritis and faster degeneration of the affected joints. It may hurt to jump into the box or posture to potty! - Scoop the box multiple times a day.
- Even with clumpable litters, dump the box at least once or twice a week.
- Wash the box weekly, rinse well, and air dry to remove any odor of the cleaning agent. Hot water and soap are best for cleaning.
- Do not use scented litter, liners, or additives like baking soda.
- If the cat likes to dig, make the litter deep. If the cat flicks the litter from his or her feet, make the litter shallow or switch to a different type (pelleted sawdust, buckwheat, etc.).
- Wash, rinse, and dry any area the cat has soiled outside the box and then use a good odor eliminator. The best ones help to enzymatically break down urine compounds and make some odorants too heavy to be sniffed. Do NOT use bleach or similar heavy products.
- Regardless, follow the cat around and see what that cat chooses – mimic that choice.
—Dr. Ana Valbuena
What’s Urgent and What’s an Emergency?

Do any of the following sound familiar? Or have you ever contemplated what you would do if your pet became ill or injured when your primary care clinic is unavailable?
- Winnie cut her paw at the dog park. It is not a large cut but looks pretty deep and is bleeding quite a bit. Medical District Vet Clinic is closed or, unfortunately, fully booked. What do I do?
- Tiger has not been eating for the past three days. Now it’s Friday night and I am off work and would like her examined as I am getting worried. Where should I take her?
- Bowie has not urinated in over 8 hours. He is in and out of the litter box, trying to pee. Where should I go?
I am sure many of you have had similar questions and or situations. Fortunately, multiple options exist for care when you can’t bring your pet to a primary care clinic. To help our clients, we have created handouts listing options for emergency clinics and specialty hospitals in Chicago.
In this blog, I want to help explain the difference between the urgent care and emergency clinics here in the Chicago area and when I would recommend going where.
After-Hours Care Options
Urgent care facilities would typically not be set up to perform surgery or hospitalize overnight but could handle most cases of pet illness. Most cases can be treated as outpatient. If not, urgent care facilities may recommend transfer to a specialty emergency clinic.
Non-specialty emergency clinics are typically open 24 hours and have varied capabilities when it comes to both diagnostics and doctor capabilities. They can handle most emergencies, but do not have the luxury of referring to or consulting with a specialist on staff. In severe cases, they may recommend referral. If your pet is very ill, I suggest that you ask them about referral to a specialty hospital.
Specialty/emergency hospitals will have the capability of performing the most advanced diagnostics and have the benefit of specialty referral when needed. These hospitals have board-certified veterinary specialists, who have 4 to 6 years of specialty training beyond veterinary school.
Think about human medicine and all the specialties. Veterinary medicine is not quite as specialized. Still, our specialties include ophthalmology, surgery, oncology, internal medicine, dermatology, dentistry, radiology, emergency and critical care, and more. These doctors often work with the most complicated, severe cases of illness and disease and manage the cases while hospitalized.
What’s the Cost?
How much do these hospitals cost? I am sure many of you are contemplating this question.
First, I want to point out that Medical District Vet Clinic is not associated with any urgent care or specialty hospitals in Chicago. For this reason, I have limited knowledge of fees. If we refer a case from our clinic directly to an ER/specialty hospital, they will often give a rough estimate.
From my experience with the specialty hospitals and emergency clinics in Chicagoland, I would say they are similarly priced. However, in some cases, the (non-specialty) emergency clinics seem to be more expensive than the specialty hospitals, despite lacking specialty referral.
All these clinics should provide an estimate for care after examining your pet. Do not be afraid to speak up if the cost is out of budget. In some cases, diagnostics can be prioritized, and doctors can discuss options if their first recommendation is not financially feasible.
Dr. Sullivan’s Recommendations
Circling back to the questions posed initially:
Winnie’s cut paw: Any of the urgent or emergency clinics should be able to handle Winnie’s cut paw.
Tiger’s three days of not eating: If your cat hasn’t eaten in three days, take her to see a veterinarian. I would suggest going to an emergency clinic or specialty hospital.
Bowie’s inability to urinate: I would highly recommend a 24-hour specialty hospital. Bowie will likely need a procedure followed by a minimum of 48 hours of hospitalization. I believe the quality of care should be superior at a specialty emergency clinic and the cost similar to that of a non-specialty ER.
—Dr. Drew Sullivan
