Our Blog
Meet Your Microbes
A few months ago, I had the opportunity to represent our clinic at a conference entitled Combating Antimicrobial Resistance with Stewardship, hosted by the Chicago Department of Public Health. It was wonderful to see professionals in all different sorts of medical fields come together to discuss topics that affect us all in how we manage our ever-developing love-hate relationship with these bugs that live all around and inside of us.
The average person has 38 trillion bacterial cells inside of them. These microbes are just as much of us and our pets as our very own cells. Bacteria are vital to our daily lives and the lives of our pets. Our understanding of our relationship with these little guys is constantly evolving. That’s why I feel it’s important to review some of the terminology related to the medications and practices used to manage bacteria.
Microbiome
This is a catchall word that refers to all the single-cell organisms that live in the body. The microbiome includes all bacteria, viruses, fungi, and protozoa that can be found inside and on the body of any animal. There are good bugs and bad bugs. They can affect everything from the smell of our breath to rashes on our skin.
People often think “microbiome” relates just to the digestive system, but it also includes any organ system where these little ones can live, such as the skin, reproductive systems, oral cavity, and respiratory systems. For the most part, these organisms live in harmony with the animal’s body. When there is an imbalance, however, or some of these critters take up space where they don’t belong, the result can mean illness for us and our pets.
Probiotics
A probiotic is a bacterium that has been found to improve gut health. (You may see probiotic products for people for other parts of the body, but in veterinary medicine probiotics almost exclusively relate to the GI system.)
For our dogs and cats especially, gut health is determined by stool quality. Diarrhea in a pet is often a sign that pathologic (bad) bacteria and other microorganisms have overpopulated. In these cases, introducing a good bacteria can help reestablish balanced populations of bacteria and improve stool quality.
Many veterinary studies in recent years have shown that giving a probiotic helps control diarrhea faster than giving an antibiotic. Plus, probiotics may make diarrhea less likely to return in the future.
Antibiotics
These don’t need a lot of explanation, but just so that we’re all on the same page, antibiotics are medications that kill bacteria by targeting cellular function that is specific to bacterial cells and not our cells.
There are different kinds of antibiotics, categorized by what kinds of bacteria they attack, how powerful they are, and how they work (e.g., by killing the bacteria or just keeping them from reproducing).
The discovery of antibiotics is arguably the most important discovery of modern medicine. But it is also important to note that the more we use these drugs the less effective they can get. It’s vital that veterinarians and other medical professionals be judicious with their use.
Antiseptics
These are compounds that try to kill any microbial life. They don’t have to be specific to one type of bacteria or virus. These are most often used topically on the skin or cleaning surfaces. I feel that we often skip over antiseptics and think only of antibiotics, but antiseptics can be a valuable tool in keeping our pets healthy and keeping the bad bacteria under control
Prebiotics
This term is a bit newer to many of us. For a long time, most medical professionals thought you could manage the microbiome either by trying to take away bad bugs (using antibiotics and such) or by adding probiotics. Recently, attention has turned to prebiotics, especially among dog food companies.
Prebiotics are typically non-soluble (meaning we don’t absorb them) foods that the “good” bugs in the microbiome like. It may seem a bit obvious, but it’s a lot easier to put food into dog and cat food than to put probiotics into a food. A probiotic has to be alive to perform its function, but food is food. Prebiotics give the good bacteria the fuel they need to thrive, which is easier to do than delivering living good bacteria.
So, there’s your refresher! I hope it was a lot less painless than all of the microbiology classes I had to take in veterinary school. I still shudder thinking about trying to remember which viruses have cellular membranes or whether or not certain protozoa are found in certain chambers of a cow’s stomach.
Now go have a banana-oat-kefir milk smoothie and give those little buggers a treat!
Alyssa Kritzman, DVM
Feature illustration from AdobeStock images
Maintaining Your Pet’s Dental Health

As pet owners, we all want to ensure our furry companions live long, healthy, and happy lives. One of the most important aspects of your pet’s overall health is their dental care, yet it often goes unnoticed.
Did you know that by the time most pets are just a few years old, they may already be suffering from some form of periodontal disease? This blog will explore the significance of dental health in pets, discuss the common signs and stages of periodontal disease, and offer tips on how you can help keep your pet’s teeth and gums healthy at home.
What Is Periodontal Disease?
Periodontal disease is a progressive condition that affects the tissues surrounding the teeth, including the gums, bone, and ligaments. It begins with the accumulation of plaque and tartar on your pet’s teeth, which harbor bacteria that cause inflammation and infection in the gums. If left untreated, periodontal disease can lead to tooth loss, chronic pain, and systemic infections that can affect your pet’s overall health.
There are four stages of periodontal disease:
Stage 1 – Gingivitis: In this early stage, your pet’s gums become inflamed and red. There is no permanent damage to the teeth or surrounding tissues, but if untreated, it can progress to more severe forms of the disease.
Stage 2 – Early Periodontitis: At this stage, plaque and tartar have begun to accumulate below the gumline. Gums may recede slightly, and some bone loss may occur, but the damage is still minimal.
Stage 3 – Moderate Periodontitis: This stage is characterized by significant gum recession, further bone loss, and infection. Pets may show signs of discomfort, and tooth mobility can start to become noticeable.
Stage 4 – Advanced Periodontitis: This is the most severe stage, where there is extensive gum recession, significant bone loss, and tooth instability. Pets at this stage may experience severe pain and infection that can spread throughout their body.
Common Symptoms of Periodontal Disease
Periodontal disease often develops slowly, and many pets don’t show obvious symptoms until the condition is advanced. However, there are several warning signs to watch for:
- Bad breath (halitosis)
- Red or swollen gums
- Drooling or excessive salivation
- Difficulty chewing or reluctance to eat hard food
- Loose or missing teeth
- Pawing at the mouth or face
- Changes in behavior, such as irritability or reluctance to be handled around the mouth
One critical thing to note is that many pets, especially dogs and cats, will continue eating even with significant dental pain. This makes it even more important to be proactive about your pet’s dental care since the discomfort may not always be immediately obvious.
When Does Periodontal Disease Develop in Pets?
Studies show that periodontal disease can start as early as three years of age in cats and dogs. In fact, around 80% of dogs will have some form of periodontal disease by the time they reach three years old. For cats, around 70% show signs of dental disease by the age of three.
While these numbers may seem alarming, the good news is that periodontal disease is largely preventable with regular dental care.
The Importance of Dental Health
Maintaining your pet’s dental health is about more than just preventing bad breath and tooth loss. Untreated periodontal disease can lead to significant pain, and the bacteria from infected gums can enter the bloodstream and affect vital organs like the heart, kidneys, and liver. This can lead to systemic health issues that can shorten your pet’s lifespan.
Regular dental care can prevent these complications and keep your pet pain-free, allowing them to live a longer, healthier life. Early detection and treatment of periodontal disease are key to avoiding severe complications and ensuring your pet’s comfort and well-being.
Tips for Regular Dental Care at Home
The good news is that with a little effort, you can help your pet maintain optimal dental health at home. Here are some effective ways to manage your pet’s dental hygiene:
- Brushing Your Pet’s Teeth: Brushing your pet’s teeth is one of the most effective ways to prevent plaque and tartar buildup. Aim to brush your pet’s teeth daily using a pet-safe toothbrush and toothpaste. Start slowly, allowing your pet to get used to the process, and always use products designed for pets. (Human toothpaste contains ingredients that can be harmful to animals.)
- Water Additives: Dental water additives can be a simple solution to help reduce plaque and tartar. These additives are mixed with your pet’s drinking water and can help maintain oral hygiene with minimal effort.
- Dental Chews and Treats: Many commercial dental chews are designed to help reduce plaque and tartar through chewing action. Look for products that are approved by the Veterinary Oral Health Council (VOHC) for proven effectiveness.
- Dental Toys: There are a variety of dental toys available that help massage your pet’s gums and scrape plaque off their teeth while they play. Always ensure any toy or treat can be indented with your fingernail to ensure that it is safe enough for your pet’s teeth and won’t cause fracture of any teeth.
- Healthy Diet: Providing your pet with a balanced diet can contribute to their overall health, including their oral health. Some specially formulated dental diets can help control plaque and tartar buildup.
Professional Dental Cleanings
Even with the best at-home care, your pet will still need professional dental cleanings from time to time. Veterinarians use specialized equipment to thoroughly clean the teeth and gums, removing plaque and tartar that may be hard to reach with regular brushing. Professional cleanings are usually done under anesthesia to ensure that your pet remains still and comfortable throughout the procedure.
Dental cleanings not only help treat existing periodontal disease, but they also give your veterinarian the opportunity to spot potential issues before they become more serious. For pets with significant dental disease, extractions may be necessary to prevent further pain or infection.
Conclusion
Dental health is an integral part of your pet’s overall well-being. Periodontal disease is common, but it is also preventable with regular dental care. By brushing your pet’s teeth, using water additives and dental chews, and scheduling routine professional cleanings, you can help keep your pet’s teeth and gums healthy, prevent systemic disease, and improve their quality of life. So, take charge of your pet’s dental health today, and enjoy the peace of mind that comes with knowing you’re doing everything you can to keep them happy and healthy for years to come.
– Dr. Jeanette Barragan
Cold Weather Cautions for Your Pets

With cooler temperatures approaching, it is important to take precautions to keep your pets safe and warm throughout the winter months.
Prolonged exposure to extreme cool temperatures can lead to frostbite, causing tissue damage to exposed areas, and hypothermia, a life-threatening drop in body temperature. Senior pets, along with very young pets or those with chronic illnesses, are more vulnerable. This becomes important for dogs and cats with arthritis, as cooler temperatures can lead to stiff joints and increased pain in the winter months.
At temperatures above 45°F most dogs are comfortable and safe outside for regular activities like walks and playtime. However, temperatures 45°F or below can cause discomfort in small, thin-coated, senior, immunocompromised, or ill dogs.
Frostbite and hypothermia become risks at temperatures below 32°F, especially in breeds not adapted to cold climates. At temperatures below 0°F, dogs should be allowed outside only for short bathroom breaks. Even hardy breeds can suffer frostbite and hypothermia quickly in these temperatures.
Cats are more vulnerable as temperatures drop below 32°F. Cats should remain indoors as much as possible, as even short exposure can cause frostbite or hypothermia. Frostbite risk areas include ears, tails, and paws. These areas are most susceptible to frostbite because they have less fur and are prone to freezing.
Symptoms of hypothermia include shivering, lifting paws off the ground, whining or attempting to return indoors, lethargy, stiff muscles, slow breathing, and pale or blue gums. This can be life-threatening!
Precautions for Your Dogs
Know your dog’s cold tolerance and limit time outside. Try to keep your dog indoors as much as possible while ensuring that they get enough exercise. Shorten walks in extremely cold weather and keep your dog active indoors by providing enrichment and indoor play.
Avoid shaving your dog’s coat during winter as their natural fur provides insulation. Regular brushing can also help their coat retain warmth. Dry your dog thoroughly after exposure to rain or snow to prevent them from getting cold.
Use warm, durable winter coats and jackets, especially for short-haired or small breed dogs. Booties and paw wax protects paws from ice, snow, and harmful chemicals like salt. Consider protective paw balm to help prevent cracking and irritation from cold surfaces and ice melt. Rock salt and other chemicals used to melt snow and ice can irritate your pet’s paw pads and, if licked off the paws, their mouth. Be sure to wipe all paws with a damp towel before your pet licks them. Dogs are at particular risk of salt poisoning during the winter due to the rock salt used, often from licking their paws after a walk. There are many pet-safe ice melt options available.
Antifreeze has a sweet taste that may attract animals. Choose a pet-safe antifreeze because even small amounts of antifreeze can be lethal. Clean any antifreeze spills immediately and keep it out of reach. Coolants and antifreeze made with propylene glycol are less toxic to pets.
What About Outdoor Cats?
Outdoor cats need extra care as they often roam unsupervised. If possible, bring cats indoors during extreme weather. Subzero temperatures, snowstorms, or icy conditions are too dangerous for outdoor cats, so they should be temporarily housed indoors. If housing indoors is not possible, then providing outdoor shelter is very important. Create a weatherproof, insulated shelter with an entrance just large enough for a cat. Line the shelter with straw, as straw repels moisture and provides better insulation than blankets. Cats often seek warmth under car hoods so be very cautious when starting your car in the morning.
In freezing weather, outdoor cats might struggle to find unfrozen water or sufficient prey, leading to dehydration and malnutrition. There are many ways we can help keep outdoor cats safe this winter. Outdoor cats require extra calories to maintain body heat, so proper nutrition is important. Using heated water bowls and replacing water frequently is important to prevent freezing water. Avoid metal bowls as tongues can stick to frozen surfaces.
By taking these precautions, you and your pet can stay warm and healthy this winter.
By Dr. Angélica Calderón
Precauciones Para Sus Mascotas en Climas Fríos
Con la llegada de las temperaturas frías, es importante tomar todas las precauciones adecuadas para mantener a sus mascotas seguras y abrigadas durante los meses de invierno.
La exposición prolongada a temperaturas extremadamente frías puede provocar congelación, e hipotermia, una caída de la temperatura corporal potencialmente mortal. Las mascotas mayores y las muy jóvenes o aquellas con enfermedades crónicas son más vulnerables. Esto es importante para los perros y gatos con artritis, ya que las temperaturas frías pueden provocar rigidez en las articulaciones y aumento del dolor en los huesos.

A temperaturas superiores a 45 °F, la mayoría de los perros se sienten cómodos y seguros afuera para actividades como paseos y juegos. Sin embargo, las temperaturas de 45 °F o menos pueden causar molestias en perros pequeños, de pelaje fino, mayores, inmunocomprometidos o enfermos. La congelación y la hipotermia se convierten en riesgos a temperaturas inferiores a 32 °F, especialmente en razas no adaptadas a climas fríos. Los gatos son más vulnerables cuando las temperaturas caen por debajo de los 32°F. A temperaturas inferiores a 0 °F, deje que los perros salgan solo para breves descansos para ir al baño. Incluso las razas vulnerables pueden sufrir congelación e hipotermia rápidamente con estas temperaturas. Los gatos deben permanecer en el interior el mayor tiempo posible, ya que incluso una exposición breve puede provocar congelación o hipotermia. Las áreas de riesgo de congelación incluyen orejas, colas y patas. Estas áreas son más susceptibles a la congelación porque tienen menos pelaje y son propensas a congelarse.
Los síntomas de hipotermia incluyen escalofríos, levantar las patas del suelo, gemir o intentar regresar al interior, letargo, rigidez muscular, respiración lenta y encías pálidas o azules. ¡Estos pueden poner en peligro la vida!
Precauciones Para los Perros
Conozca la tolerancia al frío de su perro y limite el tiempo que pasa afuera. Trate de mantener a su perro adentro el mayor tiempo posible, pero asegúrese de que aún haga suficiente ejercicio. Acorte las caminatas en climas extremadamente fríos y mantenga a su perro activo en el interior brindándole enriquecimiento y juego en el interior.
Evite cortar el pelo de su perro muy corto durante el invierno, ya que su pelaje natural le proporciona aislamiento. El cepillado regular también puede ayudar a que su pelaje retenga el calor. Seque bien a su perro después de exponerlo a la lluvia o la nieve para evitar que se enfríe.
Utilice abrigos y chaquetas de invierno cálidos y duraderos, especialmente para perros de pelo corto o de razas pequeñas. Los botines y la cera para patas protegen las patas del hielo, la nieve y productos químicos como la sal. Considere utilizar un bálsamo protector para las patas para ayudar a prevenir la irritación causadas por las superficies frías y el hielo derretido. La sal de roca y otros productos químicos utilizados para derretir la nieve y el hielo pueden irritar las almohadillas de las patas de su mascota. Asegúrese de limpiar todas las patas con una toalla húmeda antes de que su mascota las lama e irrite su boca. Los perros corren un riesgo particular de intoxicación por sal durante el invierno debido a la sal de roca utilizada, casi siempre por lamerse las patas después de un paseo. Hay muchas opciones disponibles para derretir hielo apto para mascotas.
El anticongelante tiene un sabor dulce que puede atraer a los animales. Elija un anticongelante apto para mascotas, ya que el envenenamiento por anticongelante puede ser letal incluso en pequeñas cantidades. Limpie cualquier derrame de anticongelante inmediatamente y manténgalo fuera de su alcance. Los refrigerantes y anticongelantes elaborados con propilenglicol son menos tóxicos para las mascotas.
Y Los Gatos de Afuera?
Los gatos que viven afuera necesitan cuidados especiales, ya que andan sin supervisión. Si es posible, lleve a los gatos al interior durante condiciones climáticas extremas. Las temperaturas bajo cero, las tormentas de nieve o las condiciones heladas son demasiado peligrosas para los gatos que viven afuera y deben de mantenerlos temporalmente adentro. Si no es posible, es muy importante proporcionar refugio afuera. Cree un refugio aislado y resistente a la intemperie con una entrada lo suficientemente grande para un gato. Cubra el refugio con paja, ya que la paja repele la humedad y proporciona un mejor aislamiento que las cobijas. Los gatos suelen buscar calor debajo del capó de los coches, así que hay que tener mucho cuidado.
En climas helados, los gatos de afuera pueden tener dificultades para encontrar agua no congelada o presas suficientes, lo que provoca deshidratación y desnutrición. Hay muchas maneras en que podemos ayudar a mantener seguros a los gatos de afuera.
Los gatos de afuera necesitan calorías adicionales para mantener el calor corporal, por lo que una nutrición adecuada es importante. Es importante utilizar calentadores de agua y reemplazar el agua con frecuencia para evitar que se congele. Evite los tazones de metal ya que la lengua puede pegarse a las superficies congeladas.
Si toma estas precauciones, usted y su mascota podrán mantenerse abrigados y saludables este invierno.
By Dr. Angélica Calderón
Take a Peek at My ‘Other’ Workplace

As many of you know, but others may not, in January I stepped into the role of interim director of the University of Illinois Veterinary Teaching Hospital in Urbana, while continuing to serve as medical director of Medical District Veterinary Clinic here in Chicago.
Unfortunately, a nationwide search for a permanent director of the teaching hospital did not result in a successful hire. The dean of the veterinary college has asked me to stay in my interim role through 2026, and I have agreed. While I am honored to help and enjoy the work in Urbana, I also miss seeing many of you and your pets.
Over the next two years I will remain actively involved in the daily operations of the Medical District clinic. I plan to continue seeing patients one day a week in Chicago. We are in the process of hiring another veterinarian for the Chicago clinic to help manage caseload and provide more availability for your pets.
In this blog, I want to tell you a little about the teaching hospital and showcase some exciting developments there.

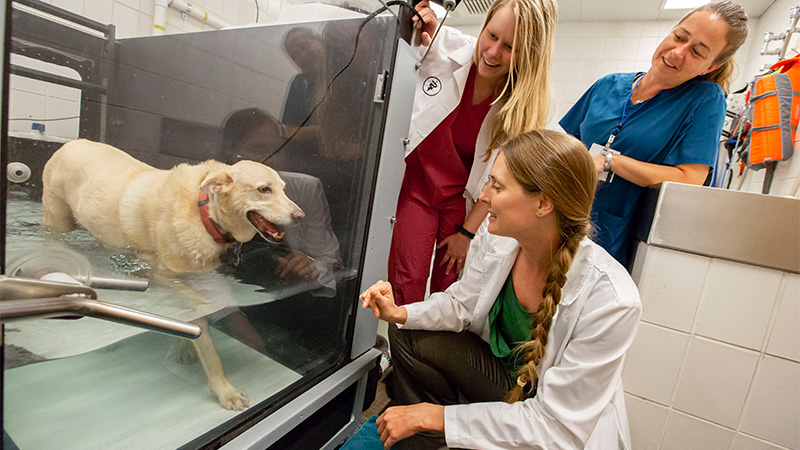




The Veterinary Teaching Hospital is a leading multi-specialty referral and emergency center, recognized nationally for its research, clinical care, and veterinary education. Organizationally within the College of Veterinary Medicine, the Medical District Veterinary Clinic is actually a satellite facility of the teaching hospital.
As interim director, I have the privilege of working alongside an exceptionally talented team of over 70 clinical faculty members and 180 support staff, across a wide range of specialties, from anesthesiology/pain management to cardiology, neurology, ophthalmology, and zoological medicine. In addition to the Medical District clinic, our facilities include the Small Animal Clinic, Large Animal Clinic, Midwest Equine, and Vet Med South Clinic.
Many features you’d expect in a human medical center can be found there:
- A linear accelerator for advanced radiation therapy
- A 3-Tesla MRI and CT scanner for high-resolution imaging
- Eight small animal surgery suites, including an interventional suite for procedures such as surgical repair of heart defects
- Advanced imaging and surgical capabilities for equine and food animal patients.
We also provide 24-hour emergency services for all domestic species, a wildlife medical clinic, rehabilitation therapy, and much more.
It’s an exciting time to be part of the teaching hospital. A new $21 million addition for our oncology service should be completed by the end of next year. This expansion will allow us to treat more animals with cancer and continue advancing cancer treatment options through research.
You might be surprised how far animal owners travel to access the resources at the University of Illinois Veterinary Teaching Hospital. They come from all across the state of Illinois, from both coasts, and even other countries! For anyone who needs advanced or specialty veterinary care, I strongly encourage looking into the options available in Urbana. Thank you for your continued support, and I look forward to seeing many of you in the clinic over the next few years.
— Dr. Drew Sullivan, Medical Director
Celebrating Veterinary Technician Week: Why CVTs and CSRs Are Vital to Your Pet’s Care

Veterinary Technician Week (October 13-19) is a time to recognize and celebrate the incredible work that certified veterinary technicians (CVTs), veterinary assistants, and customer service representatives (CSRs) do every day in the world of veterinary medicine. These professionals are the unsung heroes who ensure that your pet receives the best care possible, and they play a critical role in the smooth operation of any veterinary clinic, including ours.
The Role of Veterinary Technicians
Veterinary technicians are much more than “pet nurses.” They are highly skilled professionals trained to perform a wide range of duties, from drawing blood and running lab tests to assisting in surgeries, administering medications, and providing emergency care. They act as the veterinarian’s second set of hands, ensuring procedures run smoothly and your pet is comfortable throughout the visit.
Vet techs also provide invaluable support to pet owners. They take the time to explain medical treatments, show you how to administer medications at home, and often become trusted partners in your pet’s long-term care. Their knowledge, experience, and compassion make them essential to the success of every veterinary clinic.
The Importance of Customer Service Representatives
Customer service representatives are often the first and last point of contact when you visit our clinic. They greet you with a smile, help schedule appointments, answer questions, and ensure the check-in and check-out process is seamless. They help manage the flow of the clinic and help keep everything organized, so the veterinary team can focus on providing the best possible care for your pets.
A great CSR can make a stressful visit easier by offering clear communication, empathy, and exceptional service. They are the glue that holds the front office together, helping to create a warm, welcoming environment for both pets and their people.

How You Can Show Your Appreciation
During Veterinary Technician Week, consider taking a moment to show appreciation for the veterinary staff that care for your pets. Here are a few simple but meaningful ways to express your gratitude:
- Say Thank You: A heartfelt “thank you” can go a long way in making someone’s day. Whether it’s in person, over the phone, or in a follow-up email, acknowledging their hard work is always appreciated.
- Leave a Positive Review: Many people read online reviews before choosing a veterinary clinic. By sharing your positive experiences, you’re not only recognizing the staff but also helping future pet owners find quality care.
- Spread the Word on Social Media: If your vet tech or CSR has gone above and beyond for your pet, share your experience on social media during Veterinary Technician Week! It’s a great way to celebrate them and spread the word about the essential role they play.
- Respect Their Time: Veterinary teams work incredibly hard, often managing a heavy caseload while maintaining the highest standard of care. Being on time for your appointments, following post-care instructions, and showing patience when things get busy can go a long way in showing your appreciation.
Veterinary technicians and CSRs are the heartbeat of our clinic. We are so grateful for their tireless work and compassionate care, and we know you are too! Let’s make this Veterinary Technician Week a special one by celebrating their essential role in keeping our furry family members healthy and happy.
Thank you for your continued trust in our team!
– Ana Valbuena (she/her/ella), DVM
Celebrando la Semana del Técnico Veterinario: Por Qué los Técnicos Veterinarios y Representantes de Servicio al Clientes Son Vitales para el Cuidado de Tu Mascota

La Semana del Técnico Veterinario (Octubre 13 – 19) es un momento para reconocer y celebrar el increíble trabajo que los técnicos veterinarios, asistentes veterinarios, y los Representantes de Servicio al Clientes hacen todos los días en el mundo de la medicina veterinaria. Estos profesionales son los héroes anónimos que aseguran que tu mascota reciba el mejor cuidado posible, y juegan un papel crucial en el buen funcionamiento de cualquier clínica veterinaria, incluida la nuestra.
El Rol de los Técnicos Veterinarios
Los técnicos veterinarios son mucho más que “enfermeros de mascotas.” Son profesionales altamente capacitados para realizar una amplia gama de tareas, desde extraer sangre y realizar pruebas de laboratorio hasta asistir en cirugías, administrar medicamentos y brindar atención de emergencia. Actúan como el segundo par de manos del veterinario, asegurando que los procedimientos se realicen sin problemas y que tu mascota esté cómoda durante su visita.
Los técnicos veterinarios también brindan un apoyo invaluable a los dueños de mascotas. Se toman el tiempo para explicar los tratamientos médicos, mostrarte cómo administrar los medicamentos en casa, y a menudo se convierten en una persona de confianza en el cuidado a largo plazo de tu mascota. Su conocimiento, experiencia y compasión los hacen esenciales para el éxito de cada clínica veterinaria.
La Importancia de los Representantes de Servicio al Clientes
Los Representantes de Servicio al Clientes son a menudo el primer y último punto de contacto cuando visitas nuestra clínica. Te reciben con una sonrisa, te ayudan a programar citas, responden preguntas y aseguran que el proceso de registro y salida sea fluido. Ellos gestionan el flujo de la clínica y ayudan a mantener todo organizado, para que el equipo veterinario pueda enfocarse en brindar el mejor cuidado posible a tus mascotas.
Un buen coordinador de clientes puede hacer que una visita estresante sea más fácil al ofrecer una comunicación clara, empatía y un servicio excepcional. Son el pegamento que mantiene unido el trabajo de la oficina, ayudando a crear un ambiente cálido y acogedor tanto para las mascotas como para sus dueños.

Cómo Puedes Mostrar Tu Agradecimiento
Durante la Semana del Técnico Veterinario, considera tomarte un momento para mostrar tu agradecimiento al personal veterinario que cuida de tus mascotas. Aquí te damos algunas formas simples pero significativas de expresar tu gratitud:
- Di Gracias: Un sincero “gracias” puede alegrar el día de alguien. Ya sea en persona, por teléfono o en un correo electrónico de seguimiento, reconocer su trabajo siempre es bien recibido.
- Deja una Reseña Positiva: Muchas personas leen reseñas antes de elegir una clínica veterinaria. Compartir tus experiencias positivas no solo reconoce al personal, sino que también ayuda a otros dueños de mascotas a encontrar atención de calidad.
- Comparte en Redes Sociales: Si tu técnico veterinario o coordinador de clientes ha hecho un esfuerzo adicional por tu mascota, ¡comparte tu experiencia en redes sociales durante la Semana del Técnico Veterinario! Es una excelente manera de celebrarlos y dar a conocer el rol esencial que desempeñan.
- Respeta su Tiempo: Los equipos veterinarios trabajan increíblemente duro, a menudo manejando una carga de trabajo pesada mientras mantienen el más alto estándar de atención. Llegar a tiempo a tus citas, seguir las instrucciones de cuidado y mostrar paciencia cuando las cosas se ponen ocupadas puede ser una gran muestra de aprecio.
Los técnicos veterinarios y los Representantes de Servicio al Clientes son el corazón de nuestra clínica. Estamos muy agradecidos por su incansable trabajo y atención compasiva, ¡y sabemos que tú también! Hagamos que esta Semana del Técnico Veterinario sea especial celebrando su rol esencial en mantener a nuestros queridos miembros peludos de la familia sanos y felices.
¡Gracias por seguir confiando en nuestro equipo!
– Ana Valbuena (she/her/ella), DVM
The Bureaucracy of International Pet Travel

It finally happened.
Twelve years of practice, countless patients and clients, and it finally happened: I have a client moving their family to Australia.
I’ve helped clients send pets to every other continent (except Antarctica), but never Australia. I really wish they weren’t going. They are a lovely family, and we will miss providing service to their pets. But another reason is that Australia may be the most tedious and difficult place to transport a pet.
It will take almost a full calendar year and thousands of dollars, not to mention countless blood tests, vet visits, and forms submitted, for the pets to be successfully and legally transported to Australia.
Most countries are not nearly as difficult, costly, or time-consuming as Australia. However, before you turn your furry friend into an international jet-setter, there are two government organizations that you should know about.
Animal and Plant Health Inspection Service (APHIS)

This branch of the U.S. Department of Agriculture is responsible for protecting the health and value of American agriculture and natural resources, including our personal pets. It also ensures that all animals that leave or enter our country are healthy and free of diseases. APHIS veterinarians carry out this mission by inspecting animal facilities and working in conjunction with general practice veterinarians.
When our clients prepare their pet for international travel, they come to us for the necessary paperwork, which must then be approved by APHIS veterinarians. Before the pandemic, the paperwork completed at our clinic was then taken to an APHIS office to be endorsed. During the pandemic, this process transitioned almost completely online, so now the paperwork is scanned and uploaded to the APHIS website.
That’s why we tell you that it is time-consuming for forms to be submitted and endorsed. All forms from Wisconsin and Illinois go to one APHIS office, so it can take days for their approval.
Centers for Disease and Control and Prevention (CDC)
The CDC got involved in international animal transportation more recently. When I started practicing, international travel was exclusively in the purview of APHIS. Starting this year the CDC is requiring proof of rabies vaccination and microchipping for all dogs re-entering the United States.
To be honest, I consider this form essentially a glorified rabies certificate, but it is now required for any dog coming back into the Unites States. Being a different branch of government, CDC does not have its forms approved by APHIS.
Plan Ahead
So next time you are thinking about taking your pet with you abroad, be sure to reach out to us first for guidance. Last-minute trips are difficult, if not impossible, to accommodate. However, with good planning, the process can go smoothly (despite being annoying and tedious).
—Alyssa Kritzman, DVM
Featured photo from AdobeStock
Chronic Kidney Disease in Dogs and Cats

Chronic kidney disease (CKD) is the loss of kidney function over time. We tend to see this disease in our older cats and dogs.
The kidneys have a large amount of reserve capacity to continue to do their job effectively. For that reason, clinical signs of kidney disease may not occur until 75% of kidney function has been lost. In many cases, this means that the kidneys were losing function for months to years before clinical signs became evident. That’s why routine bloodwork and urinalysis in our senior patients, even when they are feeling well, are crucial steps for making an early diagnosis.
CKD has four stages. Pets in stages I and II may not show any clinical signs of kidney disease. In later stages, pets typically experience increased thirst and urination, lethargy, weight loss, vomiting, diarrhea, signs of dehydration, and decreased appetite.
For dogs, age of onset is related to the size of the dog. In small dogs, the age of onset generally ranges between 10 and 14 years. Large dogs, however, can experience CKD as early as 7 years of age.
In cats, CKD typically occurs at age 7 or older. An estimated 30% to 40% of cats over 10 years of age are affected, and for cats over 15 years of age, the percentage affected doubles.
The Many Functions of Kidneys
Regulating hydration. In times of dehydration, the kidney responds by conserving water. In times of excess water, the kidney efficiently removes the excess to prevent dilution of the blood. As the kidneys fail, they are no longer able to do this. The result is that urine is no longer concentrated (which means too much water is lost in the urine), and pets must drink more water to stay adequately hydrated.
Balancing calcium and phosphorus. When either calcium or phosphorus become too high, there is a risk for mineralization of the tissues. As the kidneys fail, phosphorus starts to rise. Treatment for patients with CKD requires monitoring phosphorus levels and giving a prescription diet and/or medication to keep phosphorus in a normal range.
Balancing electrolytes. As the kidneys fail, they lose their ability to conserve potassium, so these values must be closely monitored. Low potassium can lead to weakness and the need for supplementation.
Regulating blood pressure. Sensors within the kidneys monitor for high blood pressure. If these sensors are damaged, there is the risk of high blood pressure, which can damage other organs. In pets with CKD, blood pressure must be closely watched.
Retaining protein. Healthy kidneys prevent protein in the blood from being lost to the urine. As the kidneys fail, protein can leak into the urine, which can worsen kidney disease.
Producing red blood cells. The kidneys are responsible for a hormone called erythropoietin, which tells the body to produce more red blood cells when they are needed. Without this hormone, anemia can occur, so packed cell volume (PCV) and hematocrit, two red blood cell parameters, must be monitored.
Managing Chronic Kidney Disease
Chronic kidney disease, unfortunately, cannot be cured. It is a progressive disease, but it can be managed. The goals of treatment include minimizing the amount of waste products in the blood, addressing any electrolyte disturbances, maintaining adequate hydration, controlling blood pressure if high, and slowing the progression of the disease.
Pets with CKD pets must always have access to fresh water. Because their kidneys cannot concentrate their urine appropriately, these pets lose a large amount of water in the large volumes of urine they produce. Therefore, they must drink a lot of water to stay hydrated.
These pets must eat a diet specially formulated for kidney disease. Kidney diets contain less protein, sodium, and phosphorus and increased omega-3 fatty acids. Introduce the new diet over a period of 7 to 10 days. Gradually increase the proportion of the kidney diet and decrease the amount of the old diet until the pet has transitioned to eating only the new diet. Kidney diets come in a variety of flavors, so if your pet develops a flavor aversion, other options can be substituted.
As the kidney disease progresses, additional treatment may be needed to support your pet. For example, your pet may need subcutaneous fluids at home, anti-emetic (anti-vomiting) drugs, appetite stimulants, phosphorus binders, medication to reduce protein loss in the urine, medication to lower blood pressure, and potassium supplementation.
Prognosis
It is difficult to predict how long a pet with CKD will live. Regular check-ups and blood and urine tests allow doctors to monitor the progression of the disease. You should also watch your pet closely to notice changes in their health and behavior. The frequency of check-ups will be determined by your veterinarian based on staging of the disease, response to any treatments implemented, and whether your pet has developed new or worsening clinical signs.
Since early detection is paramount, consider discussing blood and urine testing for your senior pet during their next visit to the veterinarian.
– Dr. Jeanette Barragan
How to Protect Your Pets from the Heat This Summer

Summer is a fantastic time to enjoy the outdoors with your pets, but the heat can pose serious risks to their health. High temperatures can lead to dehydration, heat stroke, and even burns from hot surfaces. Here are some essential tips to help you keep your furry friends safe and comfortable during the scorching summer months.
1. Hydration Is Key
Ensure your pets always have access to fresh, cool water. Consider placing multiple water bowls around your home and yard and check them frequently to make sure they are full. Cats usually prefer running water, so consider purchasing a water fountain. For outdoor activities, bring a portable water bottle and bowl so your pet can drink on the go.
2. Avoid the Heat of the Day
Plan your walks and outdoor playtime for early morning or late evening when temperatures are cooler. The midday sun can be intense and dangerous, increasing the risk of heat stroke and burned paw pads from hot pavement.
3. Provide Shade and Ventilation
If your pet spends time outside, make sure they have access to shaded areas. Trees, tarps, or umbrellas can provide relief from direct sunlight. For pets kept indoors, ensure your home is well-ventilated and consider using fans or air conditioning to keep the environment cool.
4. Never Leave Pets in a Parked Car
Even with the windows cracked, temperatures inside a parked car can soar to dangerous levels within minutes. Leaving your pet in a hot car can lead to severe heat stroke or death. If you need to run errands, leave your pet at home in a cool, safe environment.
5. Watch for Signs of Heat Stroke
Heat stroke is a serious condition that requires immediate attention. Symptoms include excessive panting, drooling, lethargy, vomiting, diarrhea, and collapse. If you suspect your pet is suffering from heat stroke, move them to a cool area, offer small amounts of water, and seek immediate veterinary attention.
6. Grooming and Coat Care
Regular grooming can help keep your pet’s coat free of mats and tangles, which can trap heat. However, be cautious with shaving; a pet’s coat provides protection against sunburn and helps regulate their body temperature. Consult your vet or a professional groomer for advice on the best grooming practices for your pet’s breed.
7. Cool Treats and Activities
Help your pet beat the heat with frozen treats and toys. You can make simple ice treats by freezing their favorite snacks in water or broth. Kiddie pools and sprinklers can also provide a fun way for pets to cool off while playing outdoors.
Pro tip: As always, make sure to clean the ears with a veterinary-approved ear cleaner after any water interactions to help prevent ear infections.
8. Mind Hot Surfaces
Pavement, sand, and even artificial grass can become extremely hot and burn your pet’s paws. Before taking your pet for a walk, test the surface with your hand. If it’s too hot for you to touch, it’s too hot for your pet’s paws. Stick to grassy areas or wait until the ground cools down.
9. Regular Health Check-ups
Ensure your pet is up to date with their health check-ups and vaccinations. Some conditions can make pets more vulnerable to heat, and a healthy pet is better equipped to handle the stress of hot weather.
10. Tick and Flea Prevention
Summer is the peak season for ticks and fleas, which can pose serious health risks to your pets. Use veterinarian-recommended tick and flea preventatives regularly. Check your pet’s fur and skin after outdoor activities, especially in wooded or grassy areas. Remove any ticks promptly using tweezers and consult your vet if you notice any signs of flea infestations, such as excessive scratching, red bumps, or hair loss.
By taking these precautions, you can help your pets stay safe, healthy, and happy during the summer heat. Enjoy the sunny season with your furry friends, knowing you’ve done your part to protect them from the dangers of high temperatures.
Stay cool and have a wonderful summer!
— Dr. Ana Valbuena

Cómo Proteger a tus Mascotas del Calor este Verano
El verano es un momento fantástico para disfrutar del aire libre con tus mascotas, pero el calor puede representar serios riesgos para su salud. Las altas temperaturas pueden provocar deshidratación, golpes de calor e incluso quemaduras por superficies calientes. Aquí tienes algunos consejos esenciales para ayudar a mantener a tus amigos peludos seguros y cómodos durante los calurosos meses de verano.
1. La Hidratación es Clave
Asegúrate de que tus mascotas siempre tengan acceso a agua fresca y fría. Considera colocar varios tazones de agua alrededor de tu hogar y jardín y revisarlos con frecuencia para asegurarte de que estén llenos. Los gatos suelen preferir el agua corriente, así que considera comprar una fuente de agua. Para las actividades al aire libre, lleva una botella de agua portátil y un tazón para que tu mascota pueda beber en el camino.
2. Evita el Calor del Día
Planifica tus paseos y el tiempo de juego al aire libre para temprano en la mañana o tarde en la noche cuando las temperaturas son más frescas. El sol del mediodía puede ser intenso y peligroso, aumentando el riesgo de golpes de calor y quemaduras en las patas por el pavimento caliente.
3. Proporciona Sombra y Ventilación
Si tu mascota pasa tiempo afuera, asegúrate de que tenga acceso a áreas sombreadas. Los árboles, lonas o sombrillas pueden proporcionar alivio del sol directo. Para las mascotas que se quedan en el interior, asegúrate de que tu hogar esté bien ventilado y considera usar ventiladores o aire acondicionado para mantener el ambiente fresco.
4. Nunca Dejes a las Mascotas en un Auto Estacionado
Incluso con las ventanas entreabiertas, las temperaturas dentro de un coche estacionado pueden elevarse a niveles peligrosos en minutos. Dejar a tu mascota en un coche caliente puede llevar a un golpe de calor severo o la muerte. Si necesitas hacer mandados, deja a tu mascota en casa en un entorno fresco y seguro.
5. Observa los Signos de Golpe de Calor
El golpe de calor es una condición seria que requiere atención inmediata. Los síntomas incluyen jadeo excesivo, salivación, letargo, vómitos, diarrea y colapso. Si sospechas que tu mascota está sufriendo un golpe de calor, muévela a un área fresca, ofrécele pequeñas cantidades de agua y busca atención veterinaria inmediata.
6. Cuidado y Mantenimiento del Pelaje
El aseo regular puede ayudar a mantener el pelaje de tu mascota libre de nudos y enredos, que pueden atrapar el calor. Sin embargo, ten cuidado al rasurar; el pelaje de una mascota proporciona protección contra las quemaduras solares y ayuda a regular su temperatura corporal. Consulta a tu veterinario o a un peluquero profesional para obtener consejos sobre las mejores prácticas de aseo para la raza de tu mascota.
7. Golosinas y Actividades Refrescantes
Ayuda a tu mascota a combatir el calor con golosinas y juguetes congelados. Puedes hacer golosinas sencillas congelando sus snacks favoritos en agua o caldo. Las piscinas para niños y los aspersores también pueden proporcionar una forma divertida para que las mascotas se refresquen mientras juegan al aire libre. Consejo: Como siempre, asegúrate de limpiar las orejas con un limpiador de orejas aprobado por un veterinario después de cualquier interacción con el agua para ayudar a prevenir infecciones de oído.
8. Cuidado con las Superficies Calientes
El pavimento, la arena e incluso el césped artificial pueden volverse extremadamente calientes y quemar las patas de tu mascota. Antes de sacar a tu mascota a pasear, prueba la superficie con tu mano. Si está demasiado caliente para tocarla, está demasiado caliente para las patas de tu mascota. Quédate en áreas con césped o espera hasta que el suelo se enfríe.
9. Prevención de Garrapatas y Pulgas
El verano es la temporada alta para las garrapatas y las pulgas, que pueden representar serios riesgos para la salud de tus mascotas. Usa preventivos contra garrapatas y pulgas recomendados por el veterinario regularmente. Revisa el pelaje y la piel de tu mascota después de actividades al aire libre, especialmente en áreas boscosas o con hierba. Elimina cualquier garrapata rápidamente usando pinzas finas y consulta a tu veterinario si notas cualquier signo de infestación de pulgas, como rascado excesivo, bultos rojos o pérdida de pelo.
10. Revisiones de Salud Regulares
Asegúrate de que tu mascota esté al día con sus chequeos de salud y vacunas. Algunas condiciones pueden hacer que las mascotas sean más vulnerables al calor, y una mascota saludable está mejor equipada para manejar el estrés del clima caluroso.
Tomando estas precauciones, puedes ayudar a tus mascotas a mantenerse seguras, saludables y felices durante el calor del verano. Disfruta de la temporada soleada con tus amigos peludos, sabiendo que has hecho tu parte para protegerlos de los peligros de las altas temperaturas.
¡Mantente fresco y ten un maravilloso verano!
— Dr. Ana Valbuena
La Importancia de los Cultivos de Orina en las Infecciones del Tracto Urinario y Consejos Para Prevenir

Las infecciones del tracto urinario (ITU) son una preocupación común en la medicina veterinaria. Estas infecciones pueden causar una serie de síntomas incómodos y potencialmente graves en nuestras mascotas, incluyendo micción dolorosa, aumento de la frecuencia urinaria, y en casos más severos, fiebre y letargo. Aunque los síntomas pueden sugerir una ITU, otras condiciones, como las piedras en la vejiga o las enfermedades renales, pueden presentar síntomas similares. Por eso es crucial que la mascota sea examinada por su veterinario antes de empezar tratamiento.
Para diagnosticar y tratar eficazmente una ITU, uno de los pasos más críticos es realizar un cultivo de orine. Una vez que se identifica la bacteria causante, el cultivo de orine también suministra información crucial sobre qué antibióticos serán efectivos. Algunas bacterias pueden ser resistentes a ciertos antibióticos, y el uso de un medicamento ineficaz no solo retrasa la recuperación, sino que también puede contribuir a la resistencia bacteriana.
Infecciones Crónicas o Recurrentes
En algunos casos, las infecciones urinarias pueden ser crónicas o recurrentes. Esto es especialmente común en mascotas con condiciones que predisponen a las infecciones, como la diabetes o las anormalidades anatómicas del tracto urinario.
Para estos animales, se recomienda evaluación por un veterinario por lo menos dos veces al año. Es aun mas importante los cultivos de orine regulares para estos pacientes para monitorear la efectividad del tratamiento y ajustar la terapia según sea necesario. Esta vigilancia continua ayuda a prevenir complicaciones graves y a mantener la salud a largo plazo de la mascota.
Consejos Para Prevenir ITUs
- Hidratación Adecuada: asegúrese que su mascota siempre tenga acceso a agua fresca y limpia. Nunca debe prevenir que su mascota tome más agua. Hidratación adecuada ayuda a eliminar las bacterias del tracto urinario.
- Descansos Regulares para Orinar: Permite que tu perro orine con frecuencia. Retener la orina durante períodos prolongados puede promover el crecimiento bacteriano. La regla de las cajas de arena para los gatos es una caja por gato más una extra.
- Dieta Adecuada: Una dieta equilibrada es importante para mantener la salud general y fortalecer el sistema inmunológico. Su veterinario puede aconsejar en una dieta para su mascota.
- Higiene: Mantén limpia el área genital de tu perro. Los gatos son muy buenos en mantener su propria limpieza, pero pueden tener dificultades si están sobrepeso o si tiene artritis. Recorta el pelo alrededor del área genital para evitar que las bacterias se adhieran al pelaje. Limpia la parte trasera y luego la vulva después de ir al baño.
- Mantener un Peso Saludable: Las mascotas con sobrepeso son más propensos a las ITUs. El ejercicio regular y una dieta adecuada pueden ayudar a mantener un peso saludable.
- Monitorear los Síntomas: Observa los signos de una ITU, como micción frecuente, esfuerzo, sangre en la orina o comportamiento inusual. La detección y el tratamiento tempranos pueden prevenir problemas más graves.
- Evitar el Estrés: El estrés puede debilitar el sistema inmunológico. Trata de minimizar las situaciones estresantes y proporciona un ambiente calmado y estable.
Y como nota final, vamos a estar cerrados el 19 de junio por Juneteenth. Regresamos de 7 am – 7 pm el próximo día.
– Ana Valbuena (she/her/ella), DVM
Urinary Tract Infections: Why We Culture, Tips for Prevention

Urinary tract infections (UTIs) are a common concern in veterinary medicine. These infections can cause a range of uncomfortable and potentially serious symptoms in our pets, including painful urination, increased urinary frequency, and in more severe cases, fever and lethargy. Although symptoms may suggest a UTI, other conditions, such as bladder stones or kidney disease, can present similar symptoms. This is why it is crucial that the pet is examined by a veterinarian before starting treatment.
To diagnose and effectively treat a UTI, one of the most critical steps is performing a urine culture. Once the causative bacteria are identified, the urine culture also provides crucial information about which antibiotics will be effective. Some bacteria may be resistant to certain antibiotics, and using an ineffective medication not only delays recovery but can also contribute to bacterial resistance.
Chronic or Recurrent Infections
In some cases, urinary infections can be chronic or recurrent. This is especially common in pets with conditions that predispose them to infections, such as diabetes or anatomical abnormalities of the urinary tract.
For these animals, evaluation by a veterinarian at least twice a year is recommended. Regular urine cultures are even more important for these patients to monitor treatment effectiveness and adjust therapy as needed. This continuous monitoring helps prevent serious complications and maintain the long-term health of the pet.
Tips for Preventing UTIs
- Adequate Hydration: Ensure your pet always has access to fresh, clean water. Never prevent your pet from drinking more water. Adequate hydration helps flush out bacteria from the urinary tract.
- Regular Bathroom Breaks: Allow your dog to urinate frequently. Holding urine for prolonged periods can promote bacterial growth. The rule for litter boxes for cats is one box per cat plus one extra.
- Proper Diet: A balanced diet is important to maintain overall health and strengthen the immune system. Your veterinarian can advise on a diet for your pet.
- Hygiene: Keep your dog’s genital area clean. Cats are very good at keeping themselves clean, but they may have difficulties if they are overweight or have arthritis. Trim the hair around the genital area to prevent bacteria from clinging to the fur. Wipe the rear and then the vulva after going to the bathroom.
- Maintain a Healthy Weight: Pets that are overweight are more prone to UTIs. Regular exercise and a proper diet can help maintain a healthy weight.
- Monitor Symptoms: Watch for signs of a UTI, such as frequent urination, straining, blood in the urine, or unusual behavior. Early detection and treatment can prevent more serious problems.
- Avoid Stress: Stress can weaken the immune system. Try to minimize stressful situations and provide a calm and stable environment.
And as a final note, we will be closed on June 19 for Juneteenth. We will be back from 7 am to 7 pm the next day.
– Ana Valbuena (she/her/ella), DVM
Why Should You Spay or Neuter Your Dog or Cat?

Ovariohysterectomy (Spay)
Did you know that 25% of female dogs that are not spayed develop mammary tumors? Mammary tumors are commonly diagnosed in older intact female dogs, and the incidence of the development of mammary tumors in dogs is even higher than in humans.
A spay surgery, also called an ovariohysterectomy, involves the removal of the ovaries and uterus in a female dog. Although it is an invasive surgery, it is one of the most common surgeries performed in a general practice veterinary clinic.
There are many benefits to spaying your pet, and the earlier your pet is spayed the better. Complications that may arise during a female dog’s life if she is not spayed include mammary tumors/cancer and pyometra (infection of the uterus).
Additionally, spaying a dog or cat helps reduce pet overpopulation.
Mammary Cancer Risks

As previously mentioned, during a spay the uterus and both ovaries are removed. Ovaries are the female gonads that are responsible for the production of eggs and the female sex hormones, estrogen and progesterone.
Spaying a female dog reduces her risk of developing mammary cancer. If spayed before her first heat cycle, there is almost no risk that she will develop mammary cancer. After she experiences one heat cycle, the risk goes up to 7%. And after more than one heat cycle, the risk goes up to 25%.
Most mammary tumors in dogs are diagnosed between the ages of 9 and 11 years old. Risk of this tumor type is not associated with a specific breed. Small breed dogs, however, appear to be more affected. This suggests a possible genetic component, although one has not yet been identified.
According to information from Cornell University’s Richard P. Riney Canine Health Center, 50% of mammary tumors are malignant. The only way to determine if a tumor is malignant is to remove it and send it to a histopathology laboratory for interpretation.
Mammary Cancer Signs and Diagnostics
Clinical signs of mammary tumors include swollen glands, a painful abdomen, discharge from glands, ulcers near the mammary chain, and lethargy. An easy test that can be performed at most primary care veterinary clinics is called a fine-needle aspirate. This is a non-invasive test that extracts cells from the growth so that a histopathology laboratory can determine if they are cancerous.
A biopsy is a test that is more invasive than a fine-needle aspirate but less invasive than surgical mass removal.
Surgical removal is recommended if mammary cancer is suspected. Diagnostic tests performed before surgery include blood work and chest radiographs to see if the cancer has spread. Treatment ultimately depends on the type of tumor and its behavior.
If you notice any of the clinical signs for mammary cancer in your female dog, please contact your veterinarian.
Pyometra in Dogs
A pyometra is a life-threatening bacterial infection of the uterus that is caused by hormonal changes in an intact female dog. A pyometra is most common in older intact females, but an unspayed dog of any age could get a pyometra. It can occur 1 to 2 months after a heat cycle.
There are two forms of pyometra, closed and open. An open pyometra—the most common form—is when the cervix is open and infection/discharge drains from the vulva. Clinical signs include malodorous discharge from the vulva, lack of appetite, lethargy, vomiting, and drinking an excessive amount of water. Sometimes there are no clinical signs in an open pyometra. Even so, dogs can decline rapidly if not diagnosed early.
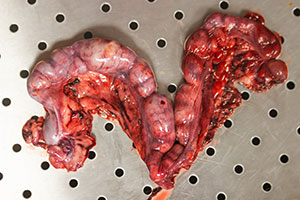
Image by Kseniia from AdobeStock.
With a closed pyometra, the cervix is closed, and the discharge/infection remains inside the uterus. The uterus can rupture in a closed pyometra, and the pet can become septic. This is a medical emergency. Pyometra can be life threatening and the treatment is an emergency spay. Pyometra can be 100% prevented if a female dog is spayed early in life.
Pyometra in Cats
Cats also get pyometra. One major difference in cats, however, is that they rarely appear sick until the very late stages of pyometra. Their abdomen can appear larger and distended due to the size of the discharge-filled uterus. Cats are seasonally polyestrous, meaning that they go into more heat cycles than dogs do, which makes them especially susceptible to getting a pyometra.
As mentioned, an ovariohysterectomy (spay) is a routine procedure performed by many general practice veterinarians. If your female cat or dog is not spayed, please reach out to your local veterinarian to discuss spaying your pet.
Castration (Neuter)
A neuter, also called a castration, involves removing both testicles in a male dog. Testes produce sperm and the male sex hormone testosterone, which is essential for the function of the prostate.
Problems that can arise if a male dog is not neutered include benign prostatic hyperplasia (BPH), prostatitis (infection of the prostate), and testicular cancer. Various studies have shown that neutering a male dog can also help with mounting behavior, inappropriate elimination, and aggression.

Like a spay, a neuter is also a routine procedure and can be performed by most primary care veterinarians. Cats are often neutered under just sedation; the procedure can take less than 5 minutes in cats.
It is highly recommended to neuter your pet after 6 months of age. There is, however, controversy in regard to large breed dogs and bone growth/development. Neutering a large breed dog early has been shown to affect bone growth and lead to joint issues in the future. In a shelter setting, pets are usually neutered at an earlier age to make them more adoptable.
If your male dog/cat is not neutered, please reach out to your local veterinarian to discuss surgery.
Benign Prostatic Hyperplasia (BPH)
Over the course of an intact male dog’s life, the prostate gland gradually enlarges due to the constant hormonal secretion. As an intact male dog ages, the prostate continues to enlarge and that can lead to discomfort/pain. This condition, called BPH, can ultimately interfere with defecation and urination.
Clinical signs of BPH include blood in the urine, difficulty urinating/defecating, and incontinence. An enlarged prostate can often be detected during a rectal exam. These signs however are very nonspecific and can resemble other medical conditions, such as a urinary tract infection, bladder stones, bladder crystals, or bladder tumor.
Neutering a male dog causes the prostate to shrink due to decreased hormonal secretion, which resolves BPH. If a dog has BPH, he will likely need anti-inflammatories and pain medications until surgical removal of the testicles. Ultimately, removing the testicles (neutering) is the treatment of choice.
Testicular Cancer
Testicular tumors are the most common genital tumors found in intact male dogs. Most testicular tumors are malignant, which means they have the potential to spread to other parts of the body.
Testicular tumors usually occur in older dogs, with an average age of 10 years old. The tumors can grow on one or both testicles. Clinical signs include asymmetric testicles, pain near groin, testicular swelling, and visibly larger testicle/testicles. Other signs include poor appetite, weight loss, and lethargy.
Treatment of choice is neutering the pet. Depending on the type of cancer, further treatment such as radiation or chemotherapy might be needed. Diagnostics, including blood work and chest radiographs to check for cancer spread, are performed before surgery.
Neutering your pet eliminates the risk of testicular cancer. If your male dog is intact and you would like to schedule a neuter surgery, please reach out to your veterinarian.
Cystine Crystals/Stones
The amino acid cystine can be excreted in the urine and can lead to the formation of bladder and kidney stones. Although cystine crystals and stones are rare, they are influenced by the presence of sex hormones. These types of crystals and stones are common in intact male dogs and require surgical removal.
Clinical signs may include straining to urinate, blood in the urine, and frequent urination episodes. Due to the anatomical difference in males and females, urinary obstruction is more common in males and it is a medical emergency.
Please reach out to your local veterinarian to further discuss spaying and neutering your pet, as there are many great benefits and various complications can be avoided if performed at an early age.
By Dr. Angélica Calderón
Images of Medical District staff and patients by Veronica
Por qué deberías esterilizar y castrar a tu perro/gato?

Ovariohisterectomía (esterilización)
Sabías que el 25% de las perras que no están esterilizadas desarrollan tumores mamarios? Los tumores mamarios se diagnostican comúnmente en perras mayores intactas y la incidencia del desarrollo de tumores mamarios en perros es incluso mayor que en humanos.
Una cirugía de esterilización, también llamada ovariohisterectomía, consiste en la extirpación de los ovarios y el útero de una perra. Aunque se trata de una cirugía invasiva, se realiza con mucha frecuencia y es una de las cirugías más comunes que se realizan en una clínica veterinaria de medicina general. Hay muchos grandes beneficios de esterilizar a su mascota y cuanto antes se esterilice a su mascota, mejor. Pueden surgir varias complicaciones a lo largo de la vida de una perra si no está esterilizada. Esto incluye tumores/cáncer mamario, piometra (infección del útero) y sobrepoblación de perros/gatos si se crían y producen descendencia, especialmente en la comunidad de animales callejeros.
Cáncer de mama
Como se mencionó anteriormente, durante una esterilización se extirpan el útero y ambos ovarios. Los ovarios son las gónadas femeninas que se encargan de la producción de óvulos y de las hormonas sexuales femeninas (estrógeno y progesterona). Esterilizar a una perra puede ayudar en gran medida a reducir la posibilidad de desarrollar cáncer de mama, independientemente de la edad. Sin embargo, hay varios factores a tener en cuenta. Si una perra es esterilizada antes de su primer ciclo de celo, la probabilidad de que desarrolle cáncer de mama es de casi el 0%. Después de experimentar un ciclo de celo, ese número sube al 7%. Si una perra experimenta más de un ciclo de celo, el número sube al 25%. La mayoría de los tumores mamarios se diagnostican entre los 9 y los 11 años de edad. No hay predilección por la raza, sin embargo, los perros de razas pequeñas parecen estar más afectados, lo que sugiere un posible componente genético. Sin embargo, aún no se ha identificado una mutación genética. Según el Centro de Salud Canina Richard P. Riney de Cornell, el 50% de los tumores mamarios son malignos y la única forma de determinar si un tumor es maligno es extirparlo y enviarlo para su interpretación histopatológica.
Los signos clínicos de los tumores mamarios incluyen glándulas inflamadas, abdomen doloroso, secreción de glándulas, úlceras cerca de la cadena mamaria y letargo. Una prueba fácil que se puede realizar en la mayoría de las clínicas veterinarias de atención primaria se llama aspirado con aguja fina. Se trata de una prueba no invasiva que se realiza habitualmente para evaluar el tipo de células presentes en el crecimiento. Estas muestras se envían para su interpretación histopatológica para evaluar si el crecimiento es canceroso. Otra prueba que se puede realizar es una biopsia, que es más invasiva que un aspirado con aguja fina, pero menos invasiva que la extirpación quirúrgica de masas. La extirpación quirúrgica es la recomendación de elección si se sospecha cáncer de mama. Se realizan varios diagnósticos antes de la cirugía; Estos incluyen análisis de sangre básicos, así como radiografías de tórax para evaluar la metástasis (diseminación). El tratamiento depende, en última instancia, del tipo de tumor y de su comportamiento. Si se observa alguno de los signos clínicos mencionados anteriormente en su perra intacta, comuníquese con su veterinario local para que se realicen los siguientes pasos apropiados.
Piometra

Una piometra es una infección bacteriana del útero potencialmente mortal causada por cambios hormonales en una perra intacta. Esto es más común en hembras mayores intactas debido a los diversos ciclos de celo de que han pasado, sin embargo, una perra intacta de cualquier edad es susceptible de contraer una piometra. Esto puede ocurrir de 1 a 2 meses después de un ciclo de celo y los signos clínicos incluyen secreción maloliente de la vulva, falta de apetito, letargo, vómitos y beber una cantidad excesiva de agua. Hay dos formas de piometra, cerrada y abierta. A veces, no hay signos clínicos en una piometra abierta, sin embargo, las perras pueden decaer rápidamente si no se diagnostican a tiempo. Una piometra abierta es cuando el cuello uterino está abierto y la infección/secreción drena fuera del cuerpo fuera de la vulva. Esta es la forma más común. Con una piometra cerrada, el cuello uterino se cierra y la secreción/infección permanece dentro del cuerpo en el útero. De esta forma, el útero puede romperse y la mascota puede volverse séptica. Esto es una emergencia médica. Una piometra puede poner en peligro la vida y el tratamiento para esto es una esterilización de emergencia. Esto se puede prevenir al 100% si una perra es esterilizada a una edad temprana.
Lo mismo se aplica a las gatas, sin embargo, una diferencia importante en las gatas es que rara vez parecen enfermas hasta las últimas etapas de la piometra. Su abdomen puede parecer más grande y distendido debido al tamaño del útero lleno de secreción. Las gatas son estacionalmente poliestroles, lo que significa que entran en más ciclos de celo que las perras, lo que los hace especialmente susceptibles a contraer una piometra.
Como se mencionó, una ovariohisterectomía (esterilización) es un procedimiento de rutina realizado por muchos veterinarios de práctica general. Si tu gata o perra no está esterilizada, comunícate con tu veterinario local para hablar sobre la esterilización de tu mascota.
Castración
Una castración consiste en extirpar ambos testículos en un perro macho. Los testículos producen espermatozoides y las hormonas sexuales masculinas (testosterona), que son esenciales para la función de la próstata. Pueden surgir varios problemas si un perro macho no está castrado. Esto incluye la hiperplasia prostática benigna (HPB), la prostatitis (infección de la próstata) y el cáncer testicular. Se han realizado varios estudios que muestran que la castración de un perro macho también puede ayudar con el comportamiento de montaje, la eliminación inapropiada y la agresión. Al igual que una esterilización, una castración también es un procedimiento de rutina y puede ser realizado por la mayoría de los veterinarios de atención primaria. Los gatos a menudo son castrados bajo sedación y el procedimiento real puede tomar tan solo menos de 5 minutos en gatos. Se recomienda encarecidamente castrar a su mascota después de los 6 meses de edad, sin embargo, existe controversia con respecto a los perros de razas grandes y el crecimiento/desarrollo óseo. Se ha demostrado que la castración temprana de un perro de raza grande afecta el crecimiento óseo y provoca problemas en las articulaciones en el futuro. En un refugio, las mascotas suelen ser castradas a una edad más temprana debido a fines de adopción.
HPB (Hiperplasia Prostática Benigna)

A lo largo de la vida de un perro macho intacto, la glándula prostática se agranda gradualmente debido a la constante secreción hormonal. A medida que un perro macho intacto envejece, la próstata continúa agrandándose y eso puede provocar molestias o dolor. Esto se denomina HPB (hiperplasia prostática benigna) y, en última instancia, puede interferir con la defecación y el orine a medida que la próstata continúa agrandándose.
Los signos clínicos de la HPB incluyen sangre en la orina, dificultad para orinar/defecar e incontinencia. Sin embargo, estos signos son muy inespecíficos y pueden parecerse a otras afecciones médicas como una infección del tracto urinario, cálculos en la vejiga, cristales en la vejiga o tumor en la vejiga. La castración de un perro macho hace que la próstata se encoja debido a la disminución de la secreción hormonal cuando se extirpan los testículos, lo que en última instancia previene la HPB. Si un perro tiene HPB, es probable que necesite antiinflamatorios y analgésicos. La extirpación total de los testículos (castración) es el tratamiento de elección.
Cáncer testicular
Los tumores testiculares son los tumores genitales más comunes que se encuentran en perros machos intactos. La mayoría de los tumores testiculares son malignos, lo que significa que tienen el potencial de propagarse a otras partes del cuerpo. Los tumores testiculares suelen aparecer en perros mayores con una edad media de 10 años. Pueden crecer en uno o ambos testículos y los signos clínicos incluyen testículos asimétricos, dolor cerca de la ingle, hinchazón testicular y un testículo o testículos visiblemente más grandes. Otros signos incluyen falta de apetito, pérdida de peso y letargo.
El tratamiento de elección es la castración de la mascota. Dependiendo del tipo de cáncer, es posible que se necesite un tratamiento adicional como radiación o quimioterapia. Se realizan varios diagnósticos antes de la cirugía, como radiografías de tórax para evaluar la metástasis (diseminación) y análisis de sangre. Castrar a tu mascota eliminará el riesgo de cáncer testicular. Si tu perro macho está intacto y deseas programar una cirugía de castración, comunícate con tu veterinario.
Cristales de cistina
El aminoácido cistina puede excretarse en la orina y provocar la formación de cálculos en la vejiga y los riñones. Aunque los cristales y cálculos de cistina son raros, están influenciados por la presencia de hormonas sexuales. Este tipo de cristales y piedras son comunes en los perros machos intactos y requieren cirugía.
Los signos clínicos pueden incluir esfuerzo para orinar, sangre en la orina y episodios frecuentes de micción. Debido a la diferencia anatómica en machos y hembras, la obstrucción urinaria es más común en los machos y se trata de una emergencia médica.
Comunícate con tu veterinario local para hablar más sobre la esterilización y castración de tu mascota, ya que hay muchos beneficios y se pueden evitar varias complicaciones si se realiza a una edad temprana.
By Dr. Angélica Calderón
Images of Medical District staff and patients by Veronica
