Posts in Category: Pet Health & Wellness
COVID and Pets: An Update from the Frontline

After two long years of this pandemic, we still do not know much about pets and SARS-CoV-2 (COVID-19), but over the last few months I have learned a lot. I am writing this blog as I am isolated in my basement with COVID-19. I am thankful for the protection I have received from vaccines as I am only experiencing very mild signs.
I hope to tell you what I have learned working firsthand with the first Illinois COVID positive dog over the past few months. According to the USDA there have only been 39 Polymerase chain reaction (PCR) positive dogs within the United States. The first dog in Illinois confirmed to be positive was a patient at Medical District Veterinary Clinic and was first tested in January 2022. He was positive on PCR, and viral sequencing information was obtained at the National Veterinary Services Laboratories in Ames, Iowa.
Since that time, I have had multiple other patients that are presumptive positives. A presumptive positive is when there is detection on a PCR test, but it is not confirmed positive with either virus sequencing or evidence of virus neutralizing antibodies. Obtaining sequencing data is challenging, most likely because the dogs have low viral load and very mild clinical signs.
Other resources
- USDA case definitions: SARS-CoV-2-case-definition.pdf (usda.gov)
- USDA Confirmed cases SAR CoV-2 in US: https://www.aphis.usda.gov/aphis/dashboards/tableau/sars-dashboard
- CDC Animal guidelines: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/animals.html#:~:text=The%20virus%20can%20spread%20from,pets%2C%20livestock%2C%20and%20wildlife.
Transmission
We believe that transmission to pets is from contact with a positive human within the household. Transmission from pets to humans is considered extremely low. Due to the risk of transmission to pets, the CDC recommend avoiding close contact with pets if you are ill. The occurrence of severe illness in pets is rare, but transmission is possible. Pets presumed positive should remain isolated from other pets until clinical signs have resolved.
Clinical Signs
It is important to remember this is a human pandemic. We know that by comparing the large number of human cases of COVID 19 and the very few cases documented in pets.
I truly believe that most pets do not acquire the virus. If they do, they are typically asymptomatic or have very mild symptoms. The clinical signs I observed in these presumptive positive cases were upper respiratory signs: nasal congestion, sneezing, reverse sneezing, and gag-like cough. These signs were odd and did not fit with classic tracheobronchitis (canine cough). When I examined these dogs, they did not cough when I touched their neck to palpate their trachea, which is the typical response during a physical exam when the patient has classic canine cough.
We have seen patients with clinical signs suspected to be secondary to SARS-CoV-2 in the past 2 to 4 weeks.
Treatment
Unfortunately, there is no approved or documented treatment for COVID in dogs or cats, but in most cases, they do not need treatment. For those pets with more severe clinical signs, I have found that corticosteroids seem to provide the most relief. The brachycephalic breeds seem to have more nasal congestion and difficulty breathing. In these pets, I have started anti-inflammatory doses of steroids and they seem to respond well.
In a few of these cases, chronic rhinitis (irritation/swelling of the mucous membrane in the nose) and sneezing has lasted for weeks to months. Home care for pets is similar to home care for most human COVID-19 cases. The virus needs to run its course. Be sure your pets continue to eat and drink. You can also put the pets in the bathroom with the shower running; the warm humid air can be soothing for the upper airway.
Testing
SARS-CoV-2 testing is not widely available for dogs or cats, but most large veterinary laboratories are offering PCR testing. Antibody testing is not widely available at present. If you feel you dog or cat has signs of SARS-CoV-2 after exposure to an infected person, I recommend contacting your veterinarian.
If you are a client at Medical District Veterinary Clinic, feel free to reach out to me and I may be able to assist in testing as I am collaborating with Dr. Ying Fang, a virologist, at the University of Illinois College of Veterinary Medicine.
– Dr. Drew Sullivan
Fear Free Practices for Furry Friends

For many people, the doctor’s office can be a scary place. So it is no surprise that many pets view going to the vet with a similar fear.
Our clinic truly believes in Fear Free practices. Our goal is to limit your pet’s stress and fear and make visits with us as pleasant as possible. There are various ways that we do this, which I would like to share with you.
Treats, Teats, and More Treats!
During your pet’s visit you will notice that we like to offer treats. We have biscuits, cheese, peanut butter – like a candy store for dogs and cats! This is not only because we think your pet is adorable and we want to spoil them, but this is also a main way we like to bond with them.
Imagine if you are at the doctor and you are anxiously waiting, and then the doctor walks in and immediately offers you your favorite treat (for me, that would be some delicious baked goods) and socializes with you. You would likely feel much calmer and connected to them. This is the equivalent of what we do with your pets.
Although we have lots of treats, if you have a dog or cat that is pickier with food, please feel free to bring whatever your pet likes best. This is not uncommon, as I have seen many patients that would eat only one food.
We encourage owners to offer treats as well during visits to help make the entire experience as positive as possible. We joke that visits go best when our patients come hungry, so you may want to consider bringing your pet to see us with an empty stomach so there is plenty of space for treats!
Getting on Their Level
We want our patients to feel comfortable, so we often will sit on the ground with them. We hope that by sitting on their level they feel less intimidated and fearful, and that they see us as their “friend.” I have noticed that when I sit on the ground and spend time in the room before even beginning my exam, my patients generally seem more at ease.
Please do not feel obligated to sit with us, but if you would like to you are totally welcome!
Limit Stress from Other Pets
Many cats never leave the home except to go to the vet. They may be stressed by traveling before they even arrive.
The smells and sounds of dogs can be very scary for them, too, which is why we recently created a separate feline waiting room and exam rooms. We use all separate supplies, have tasty treats and fun toys, and have nice feline-friendly smells. In the months since we have started using this new space, I have noticed that cats overall seem much calmer and happier.
Dogs can be become upset from other pets as well. Some of the sweetest and most affectionate dogs that I have met do not get along well with other dogs. Being around other dogs is stressful for them. I personally have a dog-reactive dog, and while she loves people, other dogs make her highly anxious.
To reduce this anxiety, we have multiple tactics, such as choosing specific exam rooms and trying to limit time in the clinic and exam room, when other pets are a trigger for the patient. We also perform exams outside in an isolated area if needed.
Fear Free for Your Pet
Please let us know if your pet is reactive with other pets, or there are any other behavioral concerns, and we will work with you to formulate a plan for their visits.
I hope you can see how much we at Medical District Veterinary Clinic truly care about our amazing patients! We look forward to continuing to make their time with us as fun and enjoyable and fear free as possible!
Amber Slaughter, DVM
Dr. Grossman Reprises His Anal Sac Primer

Well, it’s been 17 months of a global pandemic and it’s the middle of a hot (UN Climate report) summer. Though much has changed since March of 2018, dogs’ anal sac health dramatically has not. Partly because I’m tired, and partly because I answer questions about this about 20 times a day, I wanted to re-run a classic of yesteryear that takes us back to times more innocent, when a postage stamp only cost 50 cents and kids couldn’t get enough of this “texting” craze. Enjoy.
Most of us in the veterinary field face a horrible dilemma. The majority of our days are filled with details and particulars that are deemed rather unfit for discussion at the dinner table, any social gathering, and anywhere outside the professional confines of the clinic. It’s always fun to talk puppies and kittens, but a great deal of what we do during the day revolve around bodily fluids (blood, feces, urine, vomit), wounds, parasites, and the selected greatest and grossest hits of infection and disease.
Anything interesting happen at work today? Yes. Most of it was gross.
So, I’d like to discuss the grossest of all things for one moment. Please feel free to put away your chocolate custard, beef stew, and bean soup, for one moment, while we explore dog and cat anal sac disease.
Cats and dogs have anal sacs located near the periphery of the anus. These sacs excrete a liquid, often when animals defecate, that mixes into their stool and gives forth a particular and specific smell akin to a garbage bag filled with a rotting animal that has been soaked in plague juice.
At times, though, the ducts that excrete the anal sac fluid can become blocked, forcing the sacs to become enlarged, uncomfortable, swollen, and irritated. Sometimes these sacs can become so blocked that they burst forth with a mixture of all of the aforementioned dinner-party unmentionables in one fell swoop. Other times they slowly leak out at convenient times and places such as Sunday morning at 5:13 a.m. on your pillow next to your head. Often, they don’t do anything but get bigger and more uncomfortable. There are times when severe stress and discomfort can cause animals to release their anal sacs all over (seemingly) everywhere in the world.
Owners complain about their dogs and cats “scooting” their back ends over the ground or that their pets are licking their back end obsessively. The clinical signs may be more vague and scary, especially for older animals who have not ever had this problem. We may find out animals straining to defecate (as the sacs block the exit of the anus), walking stiffly, uncomfortable, not interested in eating, and, in extreme cases, vomiting. I’ve seen some dogs become so affected that they scream in pain when touched and refuse to move. I’ve seen some cats stop eating or moving and refuse to go into the litter box.
Why does this happen? you ask (while not at the dinner table). There are a few common reasons:
• Anatomical irregularities that are uncontrollable: Some dogs and cats, for whatever reason, just don’t seem to have anal sacs or anal sac ducts in the right position to allow for easy release. We have seen puppies whose anal sacs fill up monthly and need help.
• An extended period when the animal’s feces are soft and unable to naturally press on the sacs to express them: When animals have parasites (such as Giardia) or chronic diarrhea due to dietary issues or underlying illnesses, we often are not thinking that during the whole of this period, their anal sacs are (metaphorically) laughing with power as they grow bigger.
• Infiltrative disease (such as cancer): This is not very common, though it can occur. The anal sacs become diseased and cancerous. It can happen in any dog, but one tends to see this more in spaniel breeds. It does not have a good prognosis, but this condition is rare. Very rare.
• Animals, especially as they get older, learn different postures to deal with changes in the body. I have seen so many cats and dogs with untreated back pain that have to posture differently to defecate, and because of this, do not seem to express their anal sacs with the same proud efficiency that they once did. As the anal sacs get worse, they become even more uncomfortable, the animals defecate less, develop chronic soft stool, and this glorious cycle continues until you have a cat or dog that is constipated and has horribly painful anal sacs.
What can you do about it?
First, express the anal sacs. This is not something one should just try at home. I am speaking for all citizens of earth, in general, by saying that you should not do this in your kitchen before the family wakes up. Partly, because the smells of putrid sub-par day-old fish byproduct mixed with armpits and feces will probably wake them up, but also I wonder if this aspect of your relationship with your pet is one you really want to explore. While some people do learn to do this at home with their animals, I personally will not do it at home on my animals. But it is possible.
Alternatively, we can express your animal’s anal sacs so you don’t have to watch, smell, see, and, in some tragic cases, taste. We have safe zones in the clinic where no one walks for fear of spraying anal sacs. Some groomers do this for you, but few do them to completion. Ask your groomer before you assume, and talk with us about how soon you should come back for a recheck. Sometimes the anal sacs can be so full and painful that sedation may be required.
Second, animals may need additional treatment, such as antibiotics or anti-inflammatories. Most bad cases of anal sacculits, anal sac impaction, or anal sac abscesses need medication and aggressive rechecks before they are not painful or affected. It’s not generally the case that medications alone will work.
Third, we must remove the cause. Are allergies causing chronic licking, which is causing the anal sacs to be inflamed? Is your animal’s diet not allowing for a normal stool texture? Do you need to add fiber to the diet? Is your dog anxious, and this anxiety manifests in back-end licking? Are there intestinal parasites present? Is there infiltrative disease? Is there a chronic infection? Is there another animal in the house that is over-grooming the affected animal? We need to fix this.
Fourth, sometimes the anal sacs need to be removed. It’s not a cheap therapy, and it is surgery. But sometimes after coming into the clinic every two weeks and having anal sac disease a constant part of their lives, some owners elect to remove them.
As a final note, most dog owners know or have heard of anal sac issues, but most cat people are thinking that this is not applicable. This problem affects many mammals. So I’m sorry to say that even the sweetest of felines has the foulest of anal sac scents. I’ve had a run, lately, of seemingly ill cats who magically became “new” cats after their anal sacs were expressed. And, for those who play with the skunks, beavers, and opossums of your neighborhood, though I’m sure you have more on your mind, also be aware. Humans have them too, but I will let you and your loved ones google that on your own on your non-work computer.
Read things from Canada, do anything related to Canada, enjoy the summer weather noticed when opening the windows after the scent of your animal’s anal sacs permeate the walls of your Chicago apartment.
Brett Grossman, DVM
Medical District Veterinary Clinic
March Vaxness?

Right now with the pandemic, I don’t think a day goes by when I’m not thinking about vaccines. Granted, a big part of my job is vaccinating your furry family members to help keep them healthy and maintain their legal status, but with most of us having “Moderna/Pfizer versus Johnson & Johnson” or “one- or two-shot protocols” swirling in our head, I’m hoping to review a little bit about vaccines and their importance while I take a break from working on my NCAA bracket.
What Is a Vaccine?
I’m sure this is common knowledge at this point, but as a reminder, a vaccine is a composite of either a dead or modified-live version of a virus or bacteria that you expose the body to so the immune system to be able to quickly build a response if or when exposed to the actual virus or bacteria in the future. (We will not worry about the newer mRNA vaccines, as at this time the veterinary field does not use them.) Using a sports analogy, you can think about vaccines as giving the immune system a little practice with a disease, so it will be ready for game day.
When Do You Booster Vaccines?
In order for a vaccine to work, the immune system needs enough exposure to build up long-term immunity. That means, when the body is exposed, it not only remembers the disease, but can build a defense quickly, before the disease causes significant illness. Sometimes you need more than one practice session to master that layup; it’s the same with the immune system. Some immune systems need more practice than others. This mostly pertains to puppies and kittens: their immune systems are less developed, so they require more practice than an older more “skilled” immune system.
Why Do Some Vaccines Last Longer Than Others?
It can get a little confusing to know how long each vaccine last for. Some vaccines, such as canine and feline distemper, can provide immunity for up to 3 years in most adult pets. Others (e.g., leptospirosis and feline leukemia) need boosters every year to maintain adequate immunity. This is because the immune system is better at remembering certain diseases than others. Some people will never forget how to shoot a free throw, but it will probably take a lot more practice to maintain that hook shot.
What Vaccines Should My Pet Have?
Ultimately, you should discuss this question with your vet. Recommendations will vary based on your pet’s lifestyle and geographical location. Here is what we currently recommend for the average dog and cat that live in Chicago:
Dogs: DAPP (Distemper virus, Adenovirus, Parvovirus, and Parainfluenza virus), Leptospirosis, Bordetella, and Rabies
Cats (indoor only): FVRCP (Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia) and Rabies
When they are current on these vaccines, your dogs’ and cats’ immune systems will be ready to fight and win on the big game day.
Let’s hope our Illini are ready to do the same! I-L-L
Alyssa Kritzman, DVM
Photos by Fred Zwicky, © Board of Trustees of the University of Illinois, and Charles Deluvio on Unsplash
The Case of the Shih Tzu That Couldn’t Pee

What’s Your Diagnosis?
This is Chang Lu, a 10-year-old Shih Tzu. Chang Lu visited Medical District Veterinary Clinic in December with a history of straining to urinate, increased frequency of urination, and bloody urine.
During her exam she was trying to urinary every few minutes and was producing small, blood-tinged urine droplets each time. Initial diagnostics included urinalysis and X-rays. Her urine revealed significant bacteria and an overabundance of white blood cells. Below are her X-rays.
What is your diagnosis?

If you diagnosed Chang Lu with urinary tract infection and urinary bladder stones (urolithiasis), then you are correct. The large egg-shaped structures should not be there. Those are large urinary calculi (stones). Below I have notated the X-ray to point out various organs.
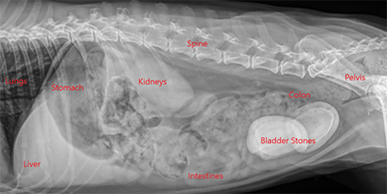
Urolithiasis (urinary bladder stones) are common in both dogs and cats. In people, most urinary stones originate in the kidneys, but in animals, more than 90% originate in the bladder, or lower urinary tract.
Urolithiasis (Urinary Bladder Stones)
Many factors, including genetic predisposition, can lead to bladder stones. Smaller breed dogs are at higher risk of developing urinary calculi (stones). Other predisposing factor include urinary tract infections, urine pH, urine mineral composition, and urine concentration.
When we see patients exhibiting the signs Chang Lu came in with (inappropriate urination, bloody urine, straining to urinate, increased frequency of urination), the most likely cause in dogs is a urinary tract infection and in cats is idiopathic (stress-induced) cystitis. In both species, however, it is important to rule out bladder stones, especially if urinary issues have been an ongoing problem for the pet.
To diagnose urinary bladder stones, veterinarians need to look inside the abdomen using X-rays and/or ultrasound. Seeing these stones is easier on X-rays than with ultrasound, and the number of stones can be more easily counted. Unfortunately, not all stones show up on X-rays, so ultrasound is needed to diagnose the non-radiopaque stones. Luckily, those that can’t be seen on X-ray are the much less common than those that can.
Treatment for Urinary Bladder Stones
Once stones have been diagnosed, treatment usually consists of a cystotomy (surgical removal of the stones) and treating the infection, if one is present. In some cases, prescription diets can be used to try to dissolve the stones. I personally have had great success with dissolution of stones in cats but very little to no success of dissolving stones with diet in dogs.
Chang Lu underwent a cystotomy, and two large stones were removed from her urinary bladder (see photo). At the time of surgery, we took a bacterial culture of her bladder, and the results showed that she had a resistant bacterial urinary tract infection. A resistant bacterial infection means the bacteria present in her bladder was resistant to most antibiotics, including the one she was initially prescribed. She was prescribed a new antibiotic in hopes the infection would be cleared.
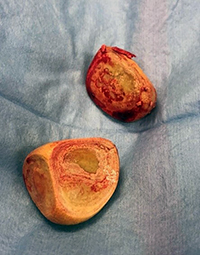
How to Prevent Urinary Bladder Stones
Once stones have been diagnosed, it is very important to identify the type of stone to understand steps that can be taken to help prevent re-occurrence. After any cystotomy, the stones are sent to the University of Minnesota Urolith Laboratory, where the stones are evaluated. Knowing the mineral composition of the stone helps veterinarians determine the best way to prevent stones in the future. In many cases, pets are started on a long-term prescription diet to help alter their urine pH, encourage urine dilution, and limit the mineral components of the diet that lead to stone formation.
Chang Lu’s stones were determined to be 100% struvite stones, most likely secondary to her resistant bacterial infection. After she finished the course of new antibiotics, her urine was re-cultured, and the infection was completely cleared. Moving forward we will be screening her urine for infection every 3 to 6 months. She has also been switched to a prescription food designed to keep new stones from forming. Chang Lu is currently doing great and all her clinical signs have resolved.
– Dr. Drew Sullivan
The ‘Why’ Behind Common Dog Vaccines

You bring your dog to the vet every year for a physical examination and vaccinations. But do you recall why your dog is receiving her shots and how her doctor has decided which ones she needs? The following is a summary of the vaccinations we offer and the diseases they prevent.
Rabies
Rabies is a virus that is contracted through the saliva (usually a bite) from an infected animal. Because rabies is always fatal and can be transmitted to humans, it is required by law that pet dogs be vaccinated. The first rabies vaccine your pet receives can be given as young as 12 weeks of age and must be re-administered one year later. Subsequent vaccines are given at either one- or three-year intervals.
DAPP, aka Distemper
This combination vaccine protects your dog from four respiratory, neurologic, and gastrointestinal viruses (distemper, adenovirus, parvovirus, and parainfluenza) that are in the environment and easy to contract through contact with an affected dog or contaminated feces. It is especially important that puppies receive this inoculation at appropriate intervals. The immune system of puppies is immature and not ready to battle these diseases. We administer this vaccine starting at 6 to 8 weeks of age, and continue every 2 to 4 weeks until your dog is at least 16 weeks of age. As your dog gets older, this vaccine will be given less frequently since his immune system is armed with antibodies to fight illness.
Leptospirosis
A bacteria found in standing water, leptospirosis is transmitted through the urine of infected rodents. A dog can contract the bacteria by drinking out of, or even walking through, a contaminated puddle. Symptoms range from mild gastrointestinal signs to liver and/or kidney failure. This potentially fatal disease is communicable to humans, so we strongly recommend all dogs receive the vaccine once a year.
There are several vaccines we give to dogs based on their lifestyles, which determines their risks.
Bordetella
Bordetella is the bacteria implicated in “kennel cough,” a respiratory illness that is easy to transmit through contact with an infected dog or through nasal or oral secretions. If your dog has contact with dogs you don’t know at a park or kennel, she should receive this vaccine. Puppies can get this vaccine as young as 6 weeks of age. It requires annual boosters.
Lyme
The Lyme disease vaccine protects dogs against the spirochete Borrelia burgdorferi, which is transmitted by ticks. Lyme disease is characterized by arthritis, lameness, fever, and rarely, a serious kidney disease. If your dog spends any time in the woods and has exposure to ticks, this vaccine is recommended. It’s worth noting that protection against ticks is an essential part of disease prevention, since Lyme is not the only disease ticks can transmit.
Canine Influenza virus
Canine flu causes fever, cough, and fatigue and can lead to life-threatening pneumonia. It’s transmitted through oral or nasal secretions or through contact with a contaminated surface. If your dog spends time around dogs you don’t know at a park or a kennel, this vaccine is an important part of disease prevention.
Vaccinations can protect your dog from contagious diseases, some of which are fatal. As your pet’s caregiver, you should understand the preventable diseases your dog is at risk for contracting. Please call our office if you have any questions about these vaccines.
Barrie Yallof, DVM
Image by Rajesh Balouria from Pixabay
The Weather Outside Is Fightful

Oh, what a typical December in a year of continual peace and normalcy.
What’s your favorite holiday memory regarding socially distanced Zoom calls with family members you haven’t seen in person for years due to splintered political realities followed by a deadly pandemic all the while keeping your 6-year-old son inside and away from his friends for 9 months and simultaneously being forced to keep an external facade of sanity and light fun in your two-holiday household while your profession, which is universally adored and undervalued at the same time, is more in demand of your time than at any other period in history?
I have so many.
So we know what usually happens here on the holiday. There is a cute blog post about keeping your dogs and cats safe, titled something like “’Tis the Wheezin’: Asthma During the Holidays.” I have written some in the past (HERE), and feel free to read. It generally can be summed up by this wise adage: “Don’t let your dog and cat eat things or get burned and remember that New Year’s Eve in Chicago generally involves people who do not have children and animals lighting off fireworks late at night to make those of us who do angry.” And don’t buy puppies, kittens, or bunnies as gifts. Instead, buy books like this inspirational tale for the animal lover in your life.
But I’m going to write about an unrelated topic: domesticated cats and the outdoors. I can imagine, even before writing this, that many people have strong feelings about this topic. My intention is not to pass judgment on anyone. I want to just give you the veterinarian perspective, and possibly give you an excuse to see photos of my fat indoor cats sitting next to holiday decorations, because that is how we indoor-cat people are generally seen and heard.

Some cats go outside. Cats go outside because some people feel that they have no choice but to let the cat out. Some people feel that it is philosophically cruel to not let the cat out, and some cats get outside by accident. All are acceptable.
I will be upfront and tell you that my two cats, Crocodile the Russian Blue mutt and Penelope the one-eyed tuxedo, do not go outside. They both try at times and have both gotten out before, but they stay inside and tolerate the complete subservience of all surrounding them.
Some of the dangers facing an outdoor cat are pretty obvious, but let’s go through them (you and I, together, like old friends who aren’t being watched):
1. Fighting with Other Cats
Cat bites and scratches are bad, cause severe infections, and can be fatal. All veterinarians have seen cats brought in with bite wounds that have become severely infected and, at worst, can puncture the abdomen, chest, eyeball, or throat and need surgical fix, hospital stays, and even euthanasia. We clean it up and give antibiotics, but it’s always concerning. This also can lead to:
2. Spread of Infectious Disease
Feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV) are spread through the exchange of bodily fluids (blood, saliva, etc.). Let’s just assume that the cats outside getting into fights are mostly ones that are homeless, and that homeless cats comprise the largest population of cats carrying these viral diseases. Well, the logic chain/train follows, and you see the danger. We can vaccinate for FeLV, so if your cat does go outside, you can get this done. There is no vaccine for FIV. And no treatment for either disease.
3. Other Infectious Disease

Rabies is a classic viral hit and can be spread through other cats or wild animals (bats, skunks, foxes). Make sure your outside cat is vaccinated for rabies, not only because it is the law but also because, even though it is rare, your sweet rabid cat can kill you and your family. (Still waiting for the Hallmark Channel’s Very Special Rabies Christmas.)
Just for fun let’s add endless respiratory infections (that can pass on to the other cats in your house), feline distemper (get your cat vaccinated for that, too), and parasitic diseases such as fleas (get monthly flea protection), ticks (get monthly tick protection), ear mites, intestinal worms (have monthly dewormers given), and ringworm.
All but one of these diseases can be passed on to you, your children, your grandparents, their friends, their friends’ neighbor, your friends’ neighbors’ son’s cat, etc. You see how this works. If you have an outdoor cat, and you’re afraid to tell your veterinarian (which you shouldn’t be), you can still take all the precautions: vaccines, preventatives, etc.
4. And Even More Infectious Disease
For the lucky, cats bring home presents, such as mice, birds, rats, etc. The rodents bring diseases and other rodents. It’s endless.
5. Cats Get Hit by Cars…
… get hit by bikers, get stuck in garages, get hurt by bad people, get snagged on fences, freeze to death, etc. [Cut to unwatchable montage of more horrible things.] It happens.
My previous cat got stuck in someone’s garage. I could not find her and searched for hours around the neighborhood. I eventually heard a cat crying in a garage and called the police who, hours later, located the owner who wasn’t on premise, to open the door. That could have easily gone another way, and I will write that fan fiction novel later.
“Lost cat” signs litter my current neighborhood, and you know they aren’t lost with a hobo bag on a train. They are all either dead, or (at best) living their lives with someone else. Also please have your outdoor cats microchipped. It’s not painful and may save your cats’ lives. You can also buy GPS trackers for their collars. I am not promoting a specific brand, but they are available anywhere.
6. Overpopulation
Cats are really good at making babies, causing the population of stray cats in the city to blow up. These cats either end up being helped by people/shelters that can barely deal with the cats they have or they are left to fend for themselves on the streets to die, starve, or spread more disease.
So first, get your outdoor cat spayed or neutered. It is absolutely the best thing for them, for their health, and to keep down the population of wild cats in need. I also do not need to explain to you how a wild tom cat will treat a sweet young lady cat taking a stroll down the promenade with her uterus and ovaries. If you want to reduce the chances that your boy cat doesn’t get into a fight, well, then neuter. There are conflicting statistics, but most sources suggest that one female cat and her mate and all the subsequent offspring amounts to 11 million cats in nine years.
7. Anti-Nature

Lastly, I fear that some of you feel like the most natural thing for the world is to let your cats outside and let them live the full entirety of their existence. I get this, I really do, but also understand how much destruction to the natural environment cats do. They destroy natural foliage and other wildlife despite their good intentions. There is some very good evidence that the best thing for “nature” is to keep your cats inside, and you can find many other resources on this topic.
There are cats that do better when they go outside. I’ve had clients keep their cats inside and later see them become anxious, yowl, not eat, urinate all over the house, etc. I don’t want your cats to suffer, but if you want to make that transition, there are things we can do. It may not be the case that your cat is anxious because it can’t go outside. In fact, it may be that it has always been anxious, but you never noticed until you kept it inside. Always have us examine your cat before making any judgments. Maybe your formerly outdoor cat is suffering from something else (UTI, pain, etc.).
As always, feel free to discuss with us at any time. This wasn’t meant to be a philosophical treatise on domesticated animals’ rights, though that is generally how I fantasize spending a great deal of my off time.
Try to relax during these times and make sure you don’t feed your dogs chocolate-covered antifreeze-infused garlic balls for the holidays, or give your cats kerosene holiday lamps for Hanukkah.
I will continue to lord over Secret Santas everywhere while I fulfill my long-standing December tradition of making holiday cookies I can’t eat in a house I don’t own.
Be safe, don’t travel, wear masks, and shop locally on-line. And Black Panther is a holiday movie.
— Brett Grossman, DVM
Aging Pets: When Is It Time to Say Goodbye?

Life with an elderly pet brings a lot of uncertainty and anxiety. We all wish for our pets to be comfortable and happy and live as long as possible, but interpreting subtle signs shown by aging pets can be challenging.
I can relate on a personal level. Our 14-year-old mixed breed dog named Oskee was diagnosed with thyroid cancer a few years ago. My wife and I did not think he would still be with us today. He has done better than expected for a dog with this diagnosis.
Oskee has been the best dog for the past 14 years. I would never want to see him have anything but a good quality of life.
Dr. Drew Sullivan
We feel very fortunate that he is doing relatively well. Recently, however, we have been noticing changes that make us wonder if this is the beginning of the end.
Facing the Inevitable
How do you know if he is uncomfortable? Is he suffering? When the time comes, how will our children react? Will we know when it is time?
These are all questions that many clients are faced with, and now my wife and I are the ones contemplating them.
When you are faced with these or similar thoughts and questions, I recommend making a list of things your pet really enjoys. For example, Oskee enjoys going for walks, chewing bones, begging/taking food from our kids. As he has aged and his condition has declined, we have seen his enjoyment in these activities decrease.
Some days he does not seem to have the energy or strength to go on much of a walk. Occasionally his legs slip out from under him. He also spends much more time sleeping and is not waiting by the dinner table like he used to. Noticing these changes helps us determine a “good” day from a “bad” day.
Focus on Quality of Life
Fortunately, his good days still outnumber the bad. An anti-inflammatory pain medication seems to make him more comfortable, and he does pretty well. I recommend clients keep a journal of good and bad days. When the bad days start outnumbering the good days, the pet’s overall quality of life needs to be considered.
For those of you with aging pets or terminally ill pets, I recommend discussing with your veterinarian what medications or therapies may help improve your pet’s overall quality of life. Unfortunately, though, most of us will be faced with a very difficult decision: when is it time to say goodbye?
It is never an easy decision. No matter how sick or old your pet is, the decision is going to be gut-wrenching and difficult. My wife and I are not looking forward to making this decision, but I owe this to Oskee when the time comes. Oskee has been the best dog for the past 14 years, and I would never want to see him have anything but a good quality of life.
Dr. Drew Sullivan
Transport a Calm Cat to the Vet

I recently came across the most amazing carrier for producing a calm cat. It’s called the Van Ness Calm Carrier. It has a sliding drawer design that allows cats in the carrier to be very easily taken out, avoids the more forceful removal from the carrier, and allows for quicker and safer unloading. I was amazed by this simple and genius idea and surprised that this carrier wasn’t more widely used.
For many cats, the only time they leave their homes and see the carrier is when they are going to the vet. They associate the carrier and the departure with being at the vet, and they begin to feel heightened stress and anxiety even before they arrive. Once we see many of these cats, it can be very difficult to handle them, and just getting them out of the carrier can be a challenge.
As a hospital that utilizes Fear Free® practices on a daily basis, we at Medical District Veterinary Clinic do our best to lessen anxiety and stress for our patients before, during, and after their visits to the vet. While the carrier choice seems simple, this important step can make a huge difference in creating a calm cat.
Below are tips to help lessen anxiety and stress for your cats when they visit with us:
- The best carriers are hard sided carriers that can be easily taken apart. In a carrier in which the top can be easily removed, more stressful and fearful cats can even be examined while they remain in the bottom half of the carrier where they are more comfortable.
- Make the carrier comfortable and enjoyable for your cat. Ideally your cat will enter the carrier on their own, and even spend time there to rest and play. To help your cat see the carrier as a happy and positive place, fill it with treats, toys, and familiar bedding that they enjoy.
- A product called Feliway® emits a synthetic feline pheromone that helps create a calming environment and reduces stress. It comes as a plug-in diffuser, spray, and wipe. Use of these products in the carrier prior to transport can be very beneficial to limit the anticipated stress and anxiety of going to the vet. We use these products all the time and see positive changes in our patients.
- Consider asking your veterinarian for a prescription medication you could administer before your cat’s visit to the clinic to serve as a mild sedative and help reduce stress and anxiety. Common medications used include gabapentin and trazodone.
By following these guidelines, you can make the experience of going to the vet much more enjoyable for feline patients—and for owners and veterinary staff as well.
—Amber Slaughter, DVM
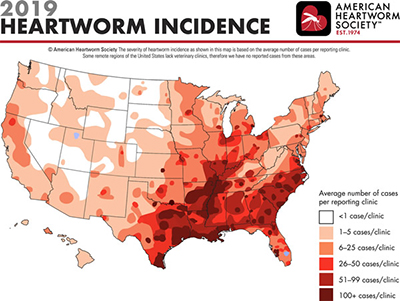
Prevention Takes the Bite Out of Heartworm Disease

Throughout this time of quarantine, I have been spending more time outside, as I am sure many of you have, too. Besides the overabundance of cicadas in my neighborhood, currently there seems to be a plethora of mosquitoes looking for a blood meal. Just as we love summer in Chicago, so do mosquitoes. Summer is the time for peak transmission of heartworm disease across the U.S. Heartworm disease is considered endemic in Illinois, and according to the American Heartworm Association, clinics in the Chicago area see an average of 25+ cases per year.
As I sit outside, I think how lucky I am because mosquitoes don’t seem to like me; my wife is not so lucky. Then I wonder if my dog, Oskee, is getting bit as much as we are? And is he getting infected with heartworms?
The importance of prevention makes so much sense once you have a little knowledge about the disease process and how monthly preventive medication works. As described in this short video, the monthly preventive does NOT prevent exposure, but kills off any immature baby heartworms already present in your dog. If the preventives are not given every 30 days, the immature heartworms can mature to juvenile worms before the next dose, thus resulting in heartworm disease.
If you miss a dose or are late giving a dose, give the dose as soon as you remember. While uncommon, an infection may develop within your dog from a single missed dose. Multiple missed doses, especially during peak transmission months, puts your dog at high risk of infection.
The heartworm test performed at annual wellness visits screens for adult heartworms. It takes 6 to 7 months after infection for the heartworms to mature into the life stage detected by the heartworm test. Therefore, if you miss a dose, start up prevention as soon as possible. Then have your dog tested within the next year to be sure that infection did not occur during the unprotected period.
For less than $10/month your pet can be protected. While there is a treatment for heartworm disease, it is more expensive and more painful than monthly prevention. The average cost of treatment for a medium-sized dog is $1,500 vs. $10/month for prevention.
If your dog is not currently on prevention or you need a refill, give us a call today. If you have questions about the different preventive medications on the market, please reach out as we would be happy to discuss your questions and concerns.
—Dr. Drew Sullivan
